444 Alaska Avenue
Suite #BAA205 Torrance, CA 90503 USA
+1 424 999 9627
24/7 Customer Support
sales@markwideresearch.com
Email us at
Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at
Corporate User License
Unlimited User Access, Post-Sale Support, Free Updates, Reports in English & Major Languages, and more
$2450
Market Overview
The UK opioids market encompasses the pharmaceutical sector’s production, distribution, and utilization of opioid medications for pain management and palliative care. Opioids are potent analgesic drugs derived from the opium poppy plant or synthesized to mimic their effects. They play a crucial role in alleviating moderate to severe pain but also pose risks of misuse, addiction, and overdose. The market’s dynamics are influenced by factors such as healthcare policies, regulatory frameworks, prescribing practices, public health initiatives, and pharmaceutical innovation.
Meaning
Opioids are a class of drugs that act on the nervous system to relieve pain. They bind to specific receptors in the brain, spinal cord, and other areas of the body, blocking pain signals and producing analgesic effects. Opioids can be natural, semi-synthetic, or synthetic compounds, with varying potency and duration of action. Common opioids include morphine, codeine, oxycodone, hydrocodone, fentanyl, and tramadol. While opioids are highly effective for managing pain, their use is associated with risks of dependence, addiction, tolerance, and adverse effects, necessitating careful prescribing and monitoring.
Executive Summary
The UK opioids market is characterized by the widespread use of opioid medications for pain management across healthcare settings. Despite their efficacy in relieving pain, opioids are subject to strict regulations and monitoring due to concerns about misuse, addiction, and overdose. The market faces challenges related to opioid prescribing practices, patient education, regulatory compliance, and access to alternative pain management therapies. However, ongoing efforts to address opioid-related harms, improve prescribing guidelines, and enhance addiction treatment services are driving initiatives to mitigate risks and promote safer opioid use.
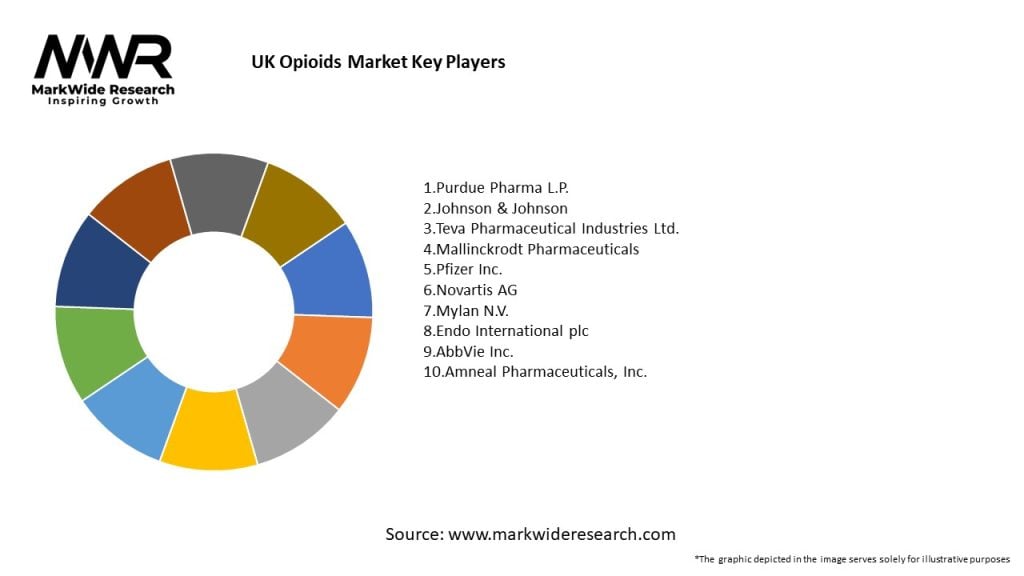
Important Note: The companies listed in the image above are for reference only. The final study will cover 18–20 key players in this market, and the list can be adjusted based on our client’s requirements.
Key Market Insights
Market Drivers
Market Restraints
Market Opportunities

Market Dynamics
The UK opioids market operates within a complex regulatory and healthcare landscape influenced by factors such as government policies, clinical guidelines, professional practices, patient preferences, and societal attitudes towards pain and addiction. These dynamics shape prescribing patterns, market trends, and access to opioid medications, impacting healthcare delivery, patient outcomes, and public health outcomes.
Regional Analysis
The UK opioids market exhibits regional variations in opioid prescribing rates, opioid-related harms, access to addiction treatment services, and healthcare infrastructure. Key regions driving market demand include urban areas with high population densities, aging demographics, and concentrations of healthcare facilities, pain clinics, and addiction treatment centers.
Competitive Landscape
Leading Companies in UK Opioids Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
Segmentation
The UK opioids market can be segmented based on various factors, including opioid class, dosage form, therapeutic indication, patient population, and distribution channel. Segmentation provides insights into market dynamics, patient preferences, prescriber practices, and emerging trends shaping opioid utilization and healthcare delivery.
Category-wise Insights
Key Benefits for Industry Participants and Stakeholders
SWOT Analysis
Market Key Trends
Covid-19 Impact
The COVID-19 pandemic has had a significant impact on the UK opioids market, influencing prescribing practices, patient access to pain management therapies, and addiction treatment services:
Key Industry Developments
Analyst Suggestions
Future Outlook
The future outlook for the UK opioids market is shaped by evolving healthcare policies, regulatory reforms, clinical practices, technological innovations, and societal attitudes towards pain and addiction. Despite ongoing challenges related to opioid misuse and overdose, there are opportunities to advance patient-centered pain management, improve access to addiction treatment services, and foster collaborations across healthcare sectors to address the complex needs of patients with pain and opioid use disorder.
Conclusion
The UK opioids market is undergoing transformational changes driven by efforts to balance the therapeutic benefits of opioids with the risks of misuse, addiction, and overdose. Healthcare stakeholders are working collaboratively to implement evidence-based practices, regulatory reforms, and public health interventions to promote safer opioid use, mitigate opioid-related harms, and improve patient outcomes. By adopting a comprehensive approach to pain management, addiction treatment, and public health policy, the UK can address the opioid epidemic while ensuring access to essential pain relief therapies for patients in need.
What is Opioids?
Opioids are a class of drugs that include both legal prescription medications and illegal substances. They are primarily used for pain relief but can also lead to addiction and other health issues.
What are the key players in the UK Opioids Market?
Key players in the UK Opioids Market include companies such as Pfizer, Johnson & Johnson, and Teva Pharmaceuticals, among others. These companies are involved in the development and distribution of various opioid medications.
What are the main drivers of the UK Opioids Market?
The main drivers of the UK Opioids Market include the increasing prevalence of chronic pain conditions, the growing aging population, and the rising demand for effective pain management solutions.
What challenges does the UK Opioids Market face?
The UK Opioids Market faces challenges such as regulatory scrutiny, the risk of addiction and overdose, and the growing public concern over opioid misuse and its consequences.
What opportunities exist in the UK Opioids Market?
Opportunities in the UK Opioids Market include the development of new formulations with lower addiction potential, advancements in pain management technologies, and increased focus on patient education and responsible prescribing practices.
What trends are shaping the UK Opioids Market?
Trends shaping the UK Opioids Market include a shift towards personalized medicine, the integration of digital health solutions for pain management, and a growing emphasis on alternative therapies to reduce reliance on opioids.
UK Opioids Market
| Segmentation Details | Description |
|---|---|
| Product Type | Morphine, Fentanyl, Oxycodone, Hydromorphone |
| Therapy Area | Chronic Pain, Cancer Pain, Postoperative Pain, Palliative Care |
| Delivery Mode | Oral, Transdermal, Injectable, Intranasal |
| End User | Hospitals, Clinics, Home Care, Pharmacies |
Please note: The segmentation can be entirely customized to align with our client’s needs.
Leading Companies in UK Opioids Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
Trusted by Global Leaders
Fortune 500 companies, SMEs, and top institutions rely on MWR’s insights to make informed decisions and drive growth.
ISO & IAF Certified
Our certifications reflect a commitment to accuracy, reliability, and high-quality market intelligence trusted worldwide.
Customized Insights
Every report is tailored to your business, offering actionable recommendations to boost growth and competitiveness.
Multi-Language Support
Final reports are delivered in English and major global languages including French, German, Spanish, Italian, Portuguese, Chinese, Japanese, Korean, Arabic, Russian, and more.
Unlimited User Access
Corporate License offers unrestricted access for your entire organization at no extra cost.
Free Company Inclusion
We add 3–4 extra companies of your choice for more relevant competitive analysis — free of charge.
Post-Sale Assistance
Dedicated account managers provide unlimited support, handling queries and customization even after delivery.
GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at