444 Alaska Avenue
Suite #BAA205 Torrance, CA 90503 USA
+1 424 999 9627
24/7 Customer Support
sales@markwideresearch.com
Email us at
Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at

Corporate User License
Unlimited User Access, Post-Sale Support, Free Updates, Reports in English & Major Languages, and more
$2750
The Middle East and Africa remote healthcare monitoring system market represents a transformative sector experiencing unprecedented growth across diverse healthcare landscapes. This dynamic market encompasses advanced technological solutions that enable continuous patient monitoring, real-time health data transmission, and remote clinical decision-making capabilities. Healthcare providers throughout the region are increasingly adopting these innovative systems to address growing patient populations, healthcare accessibility challenges, and the rising prevalence of chronic diseases.
Market dynamics indicate robust expansion driven by technological advancement, government healthcare initiatives, and increasing awareness of preventive healthcare measures. The region’s unique healthcare infrastructure challenges have created substantial opportunities for remote monitoring solutions that can bridge geographical gaps and improve patient outcomes. Digital health transformation initiatives across various countries are accelerating adoption rates, with healthcare systems recognizing the critical importance of continuous patient monitoring capabilities.
Growth trajectories suggest the market is expanding at a compound annual growth rate of 12.8%, reflecting strong demand across both public and private healthcare sectors. Technological integration with artificial intelligence, machine learning, and Internet of Things (IoT) devices is enhancing system capabilities and driving market penetration. The increasing focus on value-based healthcare models is further propelling demand for comprehensive remote monitoring solutions that demonstrate measurable patient outcomes and cost-effectiveness.
The remote healthcare monitoring system market refers to the comprehensive ecosystem of technologies, devices, and services that enable healthcare providers to monitor patient health parameters remotely through digital platforms and connected medical devices. These systems encompass wearable devices, mobile health applications, telemedicine platforms, and cloud-based data analytics solutions that facilitate continuous health monitoring outside traditional clinical settings.
Remote monitoring systems integrate various components including biosensors, wireless communication technologies, data processing platforms, and clinical decision support tools. These interconnected elements work together to collect, transmit, analyze, and interpret patient health data in real-time, enabling healthcare professionals to make informed decisions and provide timely interventions. Patient engagement is enhanced through user-friendly interfaces and mobile applications that encourage active participation in health management.
Healthcare delivery models are fundamentally transformed through these systems, shifting from reactive treatment approaches to proactive health management strategies. The technology enables continuous care coordination between patients, healthcare providers, and care teams, regardless of geographical constraints or physical limitations that might otherwise impede access to quality healthcare services.
Strategic market analysis reveals the Middle East and Africa remote healthcare monitoring system market is positioned for substantial growth, driven by increasing healthcare digitization initiatives and rising chronic disease prevalence. Key market drivers include government investments in digital health infrastructure, growing elderly populations, and the urgent need for cost-effective healthcare delivery solutions across diverse geographical regions.
Technology adoption rates are accelerating, with 65% of healthcare facilities in major urban centers implementing some form of remote monitoring capability. Market segmentation shows strong demand across multiple application areas, including cardiac monitoring, diabetes management, respiratory care, and post-operative patient surveillance. The integration of artificial intelligence and predictive analytics is enhancing system capabilities and driving healthcare provider adoption.
Competitive landscape features a mix of international technology leaders and regional healthcare solution providers, creating a dynamic ecosystem of innovation and market competition. Investment flows into healthcare technology startups and established companies are increasing, with venture capital funding growing by 28% annually. Regulatory frameworks are evolving to support digital health initiatives while ensuring patient data security and clinical efficacy standards.

Market penetration analysis reveals significant opportunities across various healthcare segments and geographical regions. Primary insights demonstrate the following critical market characteristics:
Healthcare infrastructure challenges across the Middle East and Africa region are creating substantial demand for innovative remote monitoring solutions. Geographic barriers and limited healthcare facility distribution in rural areas necessitate technology-enabled care delivery models that can reach underserved populations effectively. The growing recognition of preventive healthcare importance is driving healthcare systems to invest in continuous monitoring capabilities.
Chronic disease prevalence is increasing significantly across the region, with diabetes, cardiovascular diseases, and respiratory conditions requiring ongoing monitoring and management. Healthcare providers are recognizing that remote monitoring systems can improve patient outcomes while reducing healthcare costs through early intervention and prevention of complications. The aging population demographic trend is further amplifying demand for comprehensive monitoring solutions.
Government initiatives supporting healthcare digitization are providing policy frameworks and financial incentives for remote monitoring system adoption. Smart city developments and digital transformation strategies across various countries are incorporating healthcare technology as essential infrastructure components. Insurance coverage expansion for digital health services is removing financial barriers and encouraging broader market adoption.
Technological advancement in mobile connectivity, particularly 5G network deployment, is enabling more sophisticated and reliable remote monitoring capabilities. The proliferation of smartphone adoption and mobile internet access is creating a foundation for widespread deployment of mobile health applications and connected monitoring devices.
Infrastructure limitations in certain regions pose significant challenges to widespread remote monitoring system deployment. Internet connectivity reliability and bandwidth constraints can affect system performance and data transmission capabilities, particularly in rural and remote areas. Power supply inconsistencies and electrical grid limitations may impact device functionality and system reliability.
Regulatory complexities and varying healthcare standards across different countries create implementation challenges for system providers and healthcare organizations. Data privacy concerns and cybersecurity requirements necessitate substantial investments in security infrastructure and compliance measures. Healthcare professional training requirements for effective system utilization represent additional implementation costs and time investments.
Cultural barriers and patient acceptance challenges may limit adoption rates in certain communities where traditional healthcare delivery models are preferred. Digital literacy limitations among certain patient populations can affect system effectiveness and user engagement levels. Language diversity across the region requires localization efforts that increase system development and deployment costs.
Economic constraints and healthcare budget limitations in some countries may restrict large-scale system implementations. Currency fluctuations and economic instability can affect technology investment decisions and long-term system sustainability planning.
Emerging market segments present substantial growth opportunities for remote healthcare monitoring system providers. Maternal and child health monitoring represents an underserved market with significant potential for specialized monitoring solutions. Mental health monitoring and wellness applications are gaining recognition as essential healthcare components, creating new market categories.
Public-private partnerships are creating opportunities for large-scale system deployments supported by government healthcare initiatives. Healthcare system integration projects offer opportunities for comprehensive monitoring solution implementations across multiple healthcare facilities and networks. Medical tourism growth in the region creates demand for continuous monitoring capabilities that can support international patients.
Artificial intelligence integration opportunities are expanding system capabilities and creating new value propositions for healthcare providers. Predictive analytics and machine learning applications can enhance diagnostic accuracy and enable proactive healthcare interventions. Blockchain technology integration offers opportunities for secure health data management and interoperability solutions.
Rural healthcare expansion initiatives present opportunities for systems specifically designed for resource-constrained environments. Mobile health clinics and telemedicine programs require portable and robust monitoring solutions that can operate in challenging conditions.
Supply chain dynamics in the remote healthcare monitoring system market are characterized by complex relationships between technology manufacturers, healthcare providers, and system integrators. Component sourcing strategies are evolving to ensure reliable supply chains while managing cost pressures and quality requirements. Local manufacturing initiatives in some countries are creating opportunities for reduced costs and improved supply chain resilience.
Demand patterns show seasonal variations related to healthcare utilization trends and chronic disease management cycles. Healthcare budget allocation timing affects purchasing decisions and system deployment schedules. Technology refresh cycles create ongoing opportunities for system upgrades and capability enhancements.
Competitive dynamics are intensifying as more companies enter the market with innovative solutions and competitive pricing strategies. Market consolidation trends are emerging as larger companies acquire specialized technology providers and expand their solution portfolios. Partnership strategies between technology companies and healthcare providers are becoming increasingly important for market success.
Innovation cycles are accelerating, with new technologies and capabilities being introduced regularly. Customer expectations are evolving rapidly, requiring continuous system improvements and feature enhancements to maintain market competitiveness.
Comprehensive market analysis was conducted using multiple research methodologies to ensure accurate and reliable market insights. Primary research included extensive interviews with healthcare providers, technology vendors, and industry experts across various countries in the Middle East and Africa region. Survey methodologies were employed to gather quantitative data on system adoption rates, user satisfaction levels, and market trends.
Secondary research encompassed analysis of industry reports, government healthcare statistics, and technology adoption studies from reputable sources. Market data validation was performed through cross-referencing multiple information sources and expert verification processes. MarkWide Research analysts conducted field studies and site visits to healthcare facilities implementing remote monitoring systems.
Data collection processes included both quantitative and qualitative research approaches to capture comprehensive market dynamics. Statistical analysis methods were applied to identify trends, correlations, and market patterns. Forecasting models incorporated multiple variables including demographic trends, technology adoption rates, and economic indicators.
Quality assurance measures ensured data accuracy and reliability through multiple validation steps and expert review processes. Regional expertise was incorporated through collaboration with local market research partners and healthcare industry specialists.
Gulf Cooperation Council (GCC) countries represent the most advanced market segment, with Saudi Arabia and UAE leading in technology adoption and healthcare digitization initiatives. Government investments in smart healthcare infrastructure are driving substantial market growth, with public healthcare systems implementing comprehensive remote monitoring capabilities. Private healthcare sectors in these countries are also rapidly adopting advanced monitoring technologies.
North African markets including Egypt, Morocco, and Tunisia show strong growth potential driven by large patient populations and increasing healthcare investment. Healthcare accessibility challenges in rural areas are creating demand for remote monitoring solutions that can extend healthcare reach. Government healthcare reforms are supporting digital health initiatives and creating favorable market conditions.
Sub-Saharan Africa presents emerging opportunities with countries like South Africa, Nigeria, and Kenya leading technology adoption efforts. Mobile health initiatives are particularly successful in this region, with smartphone-based monitoring solutions gaining significant traction. International development programs and healthcare NGOs are supporting remote monitoring system deployments.
Market share distribution shows GCC countries accounting for 45% of regional adoption, while North Africa represents 30% of implementations, and Sub-Saharan Africa comprises 25% of the market. Growth rates vary significantly by country, with emerging markets showing higher percentage growth rates despite smaller absolute market sizes.
Market leadership is distributed among several key players offering diverse remote healthcare monitoring solutions. Major companies operating in the region include:
Competitive strategies focus on technology innovation, local partnerships, and comprehensive service offerings. Market differentiation is achieved through specialized applications, integration capabilities, and clinical outcome demonstrations.
Technology-based segmentation reveals diverse system categories serving different healthcare monitoring needs:
By Technology:
By Application:
By End User:
Cardiac monitoring systems represent the largest market segment, driven by high cardiovascular disease prevalence and advanced monitoring technology availability. Continuous ECG monitoring and arrhythmia detection systems are experiencing particularly strong demand from both healthcare providers and patients. Remote cardiac rehabilitation programs are expanding market opportunities beyond traditional monitoring applications.
Diabetes management solutions show exceptional growth potential, with continuous glucose monitoring adoption rates increasing rapidly across the region. Integrated insulin management systems that combine monitoring with treatment recommendations are gaining healthcare provider acceptance. Pediatric diabetes monitoring represents an emerging market segment with specialized requirements.
Respiratory monitoring applications gained significant attention following recent global health challenges, with chronic obstructive pulmonary disease (COPD) and asthma management systems showing strong adoption rates. Sleep apnea monitoring and home-based pulmonary rehabilitation programs are creating new market categories.
Maternal and fetal monitoring systems are emerging as high-growth segments, particularly in countries with expanding healthcare coverage for pregnancy care. Remote prenatal monitoring capabilities are addressing healthcare access challenges in rural areas while improving maternal health outcomes.
Healthcare providers benefit from improved patient outcomes through continuous monitoring capabilities and early intervention opportunities. Cost reduction is achieved through reduced hospital readmissions and more efficient resource utilization. Clinical decision support features enhance diagnostic accuracy and treatment effectiveness while reducing healthcare provider workload.
Patients experience enhanced convenience and improved health management through accessible monitoring technologies. Quality of life improvements result from reduced hospital visits and greater independence in health management. Early detection capabilities enable timely interventions and better long-term health outcomes.
Healthcare systems achieve improved efficiency and cost-effectiveness through optimized resource allocation and reduced emergency interventions. Population health management capabilities enable better understanding of disease patterns and healthcare needs. Data analytics provide insights for healthcare planning and policy development.
Technology providers benefit from expanding market opportunities and recurring revenue models through subscription-based services. Innovation partnerships with healthcare providers create opportunities for product development and market validation. Data monetization opportunities exist through anonymized health analytics and research collaborations.
Strengths:
Weaknesses:
Opportunities:
Threats:
Artificial intelligence integration is transforming remote monitoring capabilities through predictive analytics and automated clinical decision support. Machine learning algorithms are enabling more accurate health predictions and personalized treatment recommendations. Natural language processing is improving patient communication and system usability.
Interoperability standards are gaining importance as healthcare systems seek integrated monitoring solutions that can communicate across different platforms and devices. FHIR (Fast Healthcare Interoperability Resources) adoption is facilitating better data exchange and system integration. Cloud-based platforms are enabling scalable and flexible monitoring solutions.
Patient engagement technologies are evolving to include gamification, social features, and personalized health coaching capabilities. Mobile-first design approaches are prioritizing smartphone and tablet interfaces for better user experience. Voice-activated interfaces are emerging as important accessibility features for elderly and disabled patients.
Blockchain technology applications are being explored for secure health data management and patient consent management. Edge computing capabilities are enabling real-time data processing and reduced latency in critical monitoring applications. 5G connectivity is opening new possibilities for high-bandwidth monitoring applications and real-time video consultations.
Strategic partnerships between technology companies and healthcare providers are accelerating market development and solution deployment. Acquisition activities are consolidating market capabilities and expanding company portfolios. Investment rounds in healthcare technology startups are increasing, with venture capital funding supporting innovation and market expansion.
Regulatory approvals for new monitoring devices and platforms are expanding available solution options. Clinical validation studies are demonstrating improved patient outcomes and cost-effectiveness of remote monitoring systems. Reimbursement policy developments are improving financial accessibility of monitoring services.
Technology launches include advanced wearable devices with extended battery life and improved sensor accuracy. Platform updates are incorporating AI capabilities and enhanced user interfaces. Integration partnerships are connecting monitoring systems with electronic health records and clinical workflow systems.
Market expansion initiatives include new country entries and rural healthcare program deployments. Training programs for healthcare professionals are supporting system adoption and effective utilization. Patient education campaigns are increasing awareness and acceptance of remote monitoring technologies.
Market entry strategies should prioritize partnerships with established healthcare providers and government health agencies to ensure sustainable market penetration. MarkWide Research analysis indicates that successful companies focus on demonstrating clear clinical outcomes and cost-effectiveness to gain healthcare system acceptance. Localization efforts including language support and cultural adaptation are essential for broad market adoption.
Technology development should emphasize interoperability, user-friendly interfaces, and robust security features to meet healthcare provider requirements. Investment priorities should include AI capabilities, mobile optimization, and cloud infrastructure to support scalable growth. Clinical validation studies are crucial for establishing credibility and supporting reimbursement discussions.
Partnership strategies should include healthcare providers, technology integrators, and government agencies to create comprehensive market ecosystems. Distribution channels should leverage both direct sales and partner networks to maximize market reach. Service capabilities including training, support, and maintenance are essential for long-term customer success.
Competitive positioning should focus on specialized applications and unique value propositions rather than competing solely on price. Market timing is critical, with early entry into emerging segments providing competitive advantages. Regulatory compliance and data security should be prioritized to build trust and ensure market access.
Market growth projections indicate continued expansion driven by increasing healthcare digitization and chronic disease management needs. Technology evolution will enable more sophisticated monitoring capabilities and improved patient outcomes. Healthcare system integration will become increasingly important as monitoring becomes a standard component of care delivery.
Emerging applications in mental health monitoring, preventive care, and wellness management will create new market segments and growth opportunities. AI advancement will enable predictive healthcare capabilities and personalized treatment recommendations. Wearable technology evolution will provide more comprehensive and accurate health monitoring capabilities.
Regional development patterns suggest that GCC countries will continue leading in advanced technology adoption, while emerging markets will focus on cost-effective and accessible solutions. Government healthcare initiatives will play crucial roles in market development and technology adoption acceleration. Public-private partnerships will become increasingly important for large-scale system deployments.
Market maturation will lead to increased standardization, improved interoperability, and more comprehensive solution offerings. Competition intensity will drive innovation and cost optimization while improving overall market value propositions. Patient expectations will continue evolving, requiring continuous system improvements and feature enhancements to maintain market competitiveness and user satisfaction.
The Middle East and Africa remote healthcare monitoring system market represents a dynamic and rapidly evolving sector with substantial growth potential across diverse healthcare environments. Market fundamentals including increasing chronic disease prevalence, healthcare accessibility challenges, and government digitization initiatives create strong foundations for continued expansion and technology adoption.
Technology advancement and integration capabilities are driving system sophistication and clinical value, while cost-effectiveness demonstrations are supporting healthcare provider adoption decisions. Regional diversity creates opportunities for various solution approaches, from advanced AI-powered systems in developed markets to accessible mobile-based solutions in emerging economies. Stakeholder collaboration between technology providers, healthcare systems, and government agencies will be essential for realizing the full market potential and achieving sustainable growth in this transformative healthcare technology sector.
What is Remote Healthcare Monitoring System?
Remote Healthcare Monitoring System refers to technologies and services that enable the monitoring of patients’ health data from a distance. This includes the use of devices and applications that track vital signs, manage chronic conditions, and facilitate communication between patients and healthcare providers.
What are the key players in the Middle East and Africa Remote Healthcare Monitoring System Market?
Key players in the Middle East and Africa Remote Healthcare Monitoring System Market include Philips Healthcare, Medtronic, and Siemens Healthineers, among others. These companies are known for their innovative solutions in remote patient monitoring and telehealth services.
What are the growth factors driving the Middle East and Africa Remote Healthcare Monitoring System Market?
The growth of the Middle East and Africa Remote Healthcare Monitoring System Market is driven by increasing chronic disease prevalence, rising healthcare costs, and the growing demand for telehealth services. Additionally, advancements in technology and increased smartphone penetration are facilitating remote monitoring.
What challenges does the Middle East and Africa Remote Healthcare Monitoring System Market face?
Challenges in the Middle East and Africa Remote Healthcare Monitoring System Market include regulatory hurdles, data privacy concerns, and the need for reliable internet connectivity. These factors can hinder the widespread adoption of remote healthcare solutions.
What opportunities exist in the Middle East and Africa Remote Healthcare Monitoring System Market?
Opportunities in the Middle East and Africa Remote Healthcare Monitoring System Market include the expansion of telemedicine services and the integration of artificial intelligence in healthcare monitoring. There is also potential for growth in rural areas where access to healthcare is limited.
What trends are shaping the Middle East and Africa Remote Healthcare Monitoring System Market?
Trends in the Middle East and Africa Remote Healthcare Monitoring System Market include the increasing use of wearable devices for health tracking and the rise of mobile health applications. Additionally, there is a growing focus on personalized medicine and patient engagement through technology.
Middle East and Africa Remote Healthcare Monitoring System Market
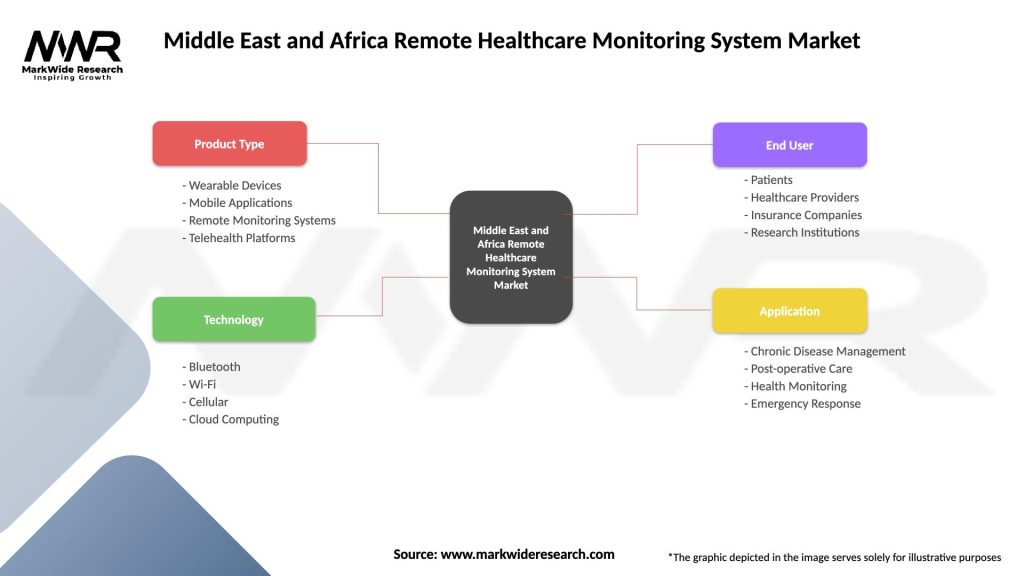
| Segmentation Details | Description |
|---|---|
| Product Type | Wearable Devices, Mobile Applications, Remote Monitoring Systems, Telehealth Platforms |
| Technology | Bluetooth, Wi-Fi, Cellular, Cloud Computing |
| End User | Patients, Healthcare Providers, Insurance Companies, Research Institutions |
| Application | Chronic Disease Management, Post-operative Care, Health Monitoring, Emergency Response |
Please note: The segmentation can be entirely customized to align with our client’s needs.
Leading companies in the Middle East and Africa Remote Healthcare Monitoring System Market
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
Trusted by Global Leaders
Fortune 500 companies, SMEs, and top institutions rely on MWR’s insights to make informed decisions and drive growth.
ISO & IAF Certified
Our certifications reflect a commitment to accuracy, reliability, and high-quality market intelligence trusted worldwide.
Customized Insights
Every report is tailored to your business, offering actionable recommendations to boost growth and competitiveness.
Multi-Language Support
Final reports are delivered in English and major global languages including French, German, Spanish, Italian, Portuguese, Chinese, Japanese, Korean, Arabic, Russian, and more.
Unlimited User Access
Corporate License offers unrestricted access for your entire organization at no extra cost.
Free Company Inclusion
We add 3–4 extra companies of your choice for more relevant competitive analysis — free of charge.
Post-Sale Assistance
Dedicated account managers provide unlimited support, handling queries and customization even after delivery.
GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at