444 Alaska Avenue
Suite #BAA205 Torrance, CA 90503 USA
+1 424 999 9627
24/7 Customer Support
sales@markwideresearch.com
Email us at
Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at
Corporate User License
Unlimited User Access, Post-Sale Support, Free Updates, Reports in English & Major Languages, and more
$3450
Market Overview
The medical simulation education market is a crucial component of healthcare training, providing immersive and interactive learning experiences for medical professionals. Utilizing simulation technology, this market offers hands-on training opportunities for healthcare practitioners to enhance their clinical skills and decision-making abilities in a safe and controlled environment. With the increasing emphasis on patient safety, medical simulation education has become an integral part of medical curricula and professional development programs worldwide.
Meaning
Medical simulation education involves the use of simulated scenarios, equipment, and environments to mimic real-life clinical situations for training purposes. It encompasses various modalities such as virtual reality, augmented reality, task trainers, and high-fidelity manikins to replicate clinical scenarios ranging from basic procedures to complex surgical interventions. Medical simulation allows learners to practice skills, refine techniques, and improve clinical competence without risking patient safety.
Executive Summary
The medical simulation education market has experienced significant growth in recent years, driven by factors such as advancements in simulation technology, increasing demand for competency-based training, and growing awareness of patient safety concerns. This market offers diverse opportunities for educational institutions, healthcare organizations, and simulation technology providers to collaborate and innovate in delivering effective training solutions. Understanding the key market insights, drivers, restraints, and dynamics is essential for stakeholders to capitalize on emerging trends and navigate the competitive landscape.

Important Note: The companies listed in the image above are for reference only. The final study will cover 18–20 key players in this market, and the list can be adjusted based on our client’s requirements.
Key Market Insights
Market Drivers
Market Restraints
Market Opportunities
Market Dynamics
The medical simulation education market operates within a dynamic ecosystem shaped by technological innovation, educational reform, regulatory requirements, and healthcare industry trends. These dynamics influence market growth, adoption rates, investment priorities, and strategic partnerships among stakeholders, requiring continuous adaptation and alignment with evolving educational needs and industry standards.
Regional Analysis
Regional variations in healthcare infrastructure, educational policies, and healthcare workforce demographics contribute to disparities in the adoption and utilization of medical simulation education:
Competitive Landscape
Leading Companies in the Medical Simulation Education Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
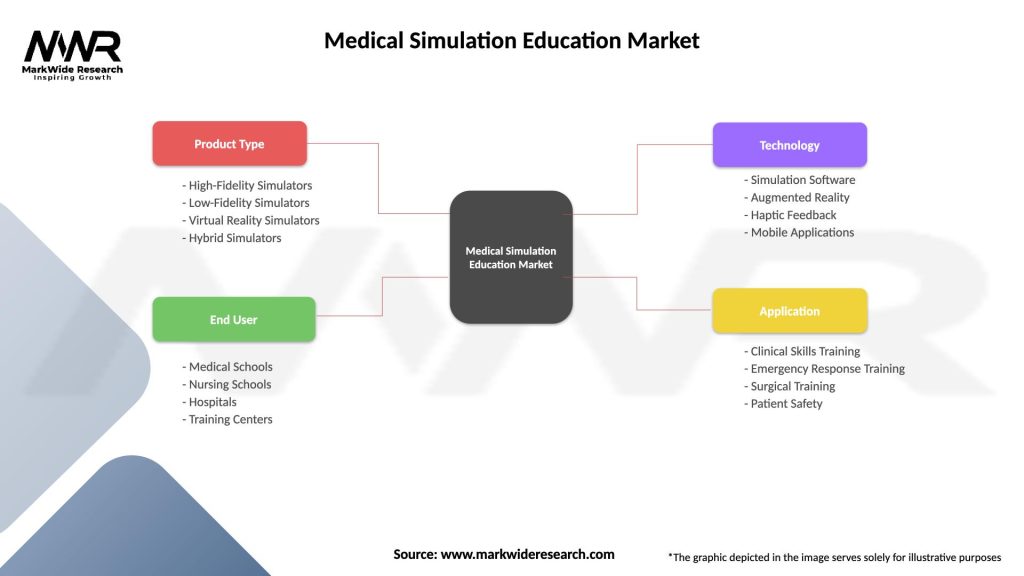
Segmentation
The medical simulation education market can be segmented based on various factors, including simulation modality, clinical specialty, learner profile, and geographic region:
Segmentation provides insights into the diverse applications, target audiences, and market opportunities within the medical simulation education landscape, guiding stakeholders in the development and delivery of tailored training solutions.
Category-wise Insights
Key Benefits for Industry Participants and Stakeholders
SWOT Analysis
A SWOT analysis of the medical simulation education market highlights key internal strengths, weaknesses, and external opportunities, and threats:
Understanding these internal and external factors helps stakeholders capitalize on strengths, address weaknesses, leverage opportunities, and mitigate threats within the medical simulation education market.
Market Key Trends
Covid-19 Impact
The COVID-19 pandemic has profoundly impacted the medical simulation education market:
Key Industry Developments
Analyst Suggestions
Future Outlook
The future of the medical simulation education market is characterized by:
Conclusion
The medical simulation education market plays a pivotal role in transforming healthcare education and training, offering immersive, safe, and effective learning experiences for healthcare professionals. With the convergence of advanced simulation technology, evidence-based pedagogy, and evolving healthcare needs, simulation-based education is poised to drive improvements in clinical competence, patient safety, and healthcare quality. By embracing innovation, collaboration, and evidence-based practice, stakeholders can harness the full potential of medical simulation to advance healthcare education and enhance patient care in the years to come.
What is Medical Simulation Education?
Medical Simulation Education refers to the use of simulated clinical environments and scenarios to train healthcare professionals. This approach enhances learning through hands-on practice, allowing students to develop skills in a safe and controlled setting.
What are the key players in the Medical Simulation Education Market?
Key players in the Medical Simulation Education Market include Laerdal Medical, CAE Healthcare, and Simulaids, among others. These companies provide a range of simulation products and services designed to improve medical training and education.
What are the growth factors driving the Medical Simulation Education Market?
The Medical Simulation Education Market is driven by the increasing demand for skilled healthcare professionals, advancements in simulation technology, and the need for effective training methods. Additionally, the growing emphasis on patient safety and quality of care contributes to market growth.
What challenges does the Medical Simulation Education Market face?
Challenges in the Medical Simulation Education Market include high initial costs of simulation equipment and the need for ongoing maintenance and updates. Additionally, there may be resistance to adopting new training methods among some educational institutions.
What opportunities exist in the Medical Simulation Education Market?
Opportunities in the Medical Simulation Education Market include the expansion of online and hybrid learning models, increased investment in healthcare education, and the development of more advanced simulation technologies. These factors can enhance training effectiveness and accessibility.
What trends are shaping the Medical Simulation Education Market?
Trends in the Medical Simulation Education Market include the integration of virtual reality and augmented reality into training programs, the use of artificial intelligence for personalized learning experiences, and a growing focus on interprofessional education. These innovations are transforming how medical training is delivered.
Medical Simulation Education Market
| Segmentation Details | Description |
|---|---|
| Product Type | High-Fidelity Simulators, Low-Fidelity Simulators, Virtual Reality Simulators, Hybrid Simulators |
| End User | Medical Schools, Nursing Schools, Hospitals, Training Centers |
| Technology | Simulation Software, Augmented Reality, Haptic Feedback, Mobile Applications |
| Application | Clinical Skills Training, Emergency Response Training, Surgical Training, Patient Safety |
Please note: The segmentation can be entirely customized to align with our client’s needs.
Leading Companies in the Medical Simulation Education Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
North America
o US
o Canada
o Mexico
Europe
o Germany
o Italy
o France
o UK
o Spain
o Denmark
o Sweden
o Austria
o Belgium
o Finland
o Turkey
o Poland
o Russia
o Greece
o Switzerland
o Netherlands
o Norway
o Portugal
o Rest of Europe
Asia Pacific
o China
o Japan
o India
o South Korea
o Indonesia
o Malaysia
o Kazakhstan
o Taiwan
o Vietnam
o Thailand
o Philippines
o Singapore
o Australia
o New Zealand
o Rest of Asia Pacific
South America
o Brazil
o Argentina
o Colombia
o Chile
o Peru
o Rest of South America
The Middle East & Africa
o Saudi Arabia
o UAE
o Qatar
o South Africa
o Israel
o Kuwait
o Oman
o North Africa
o West Africa
o Rest of MEA
Trusted by Global Leaders
Fortune 500 companies, SMEs, and top institutions rely on MWR’s insights to make informed decisions and drive growth.
ISO & IAF Certified
Our certifications reflect a commitment to accuracy, reliability, and high-quality market intelligence trusted worldwide.
Customized Insights
Every report is tailored to your business, offering actionable recommendations to boost growth and competitiveness.
Multi-Language Support
Final reports are delivered in English and major global languages including French, German, Spanish, Italian, Portuguese, Chinese, Japanese, Korean, Arabic, Russian, and more.
Unlimited User Access
Corporate License offers unrestricted access for your entire organization at no extra cost.
Free Company Inclusion
We add 3–4 extra companies of your choice for more relevant competitive analysis — free of charge.
Post-Sale Assistance
Dedicated account managers provide unlimited support, handling queries and customization even after delivery.
GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at