444 Alaska Avenue
Suite #BAA205 Torrance, CA 90503 USA
+1 424 999 9627
24/7 Customer Support
sales@markwideresearch.com
Email us at
Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at
Corporate User License
Unlimited User Access, Post-Sale Support, Free Updates, Reports in English & Major Languages, and more
$3450
Market Overview
Healthcare fraud analytics is a rapidly growing sector within the healthcare industry. As healthcare costs continue to rise, the need for effective fraud detection and prevention measures becomes increasingly crucial. Healthcare fraud refers to the deliberate act of deceiving or misrepresenting information for financial gain in the healthcare system. Fraudulent activities can include billing for services not provided, falsifying medical records, and engaging in kickback schemes, among others.
Meaning
Healthcare fraud analytics involves the use of advanced data analytics techniques and technologies to identify patterns and anomalies in healthcare data that may indicate fraudulent activities. By analyzing large volumes of healthcare data, such as claims data, patient records, and provider information, healthcare organizations can uncover potential fraud cases and take appropriate actions to mitigate risks and prevent financial losses.
Executive Summary
The healthcare fraud analytics market has experienced significant growth in recent years, driven by the increasing prevalence of healthcare fraud and the growing adoption of advanced analytics solutions by healthcare organizations. The market offers a range of software and services specifically designed to detect, investigate, and prevent fraud in the healthcare sector. These solutions leverage machine learning algorithms, artificial intelligence, and predictive modeling techniques to identify suspicious patterns and outliers in healthcare data.
Important Note: The companies listed in the image above are for reference only. The final study will cover 18–20 key players in this market, and the list can be adjusted based on our client’s requirements.
Key Market Insights
Market Drivers
Several factors are driving the growth of the healthcare fraud analytics market:
Market Restraints
Despite the promising growth prospects, the healthcare fraud analytics market faces certain challenges:
Market Opportunities
The healthcare fraud analytics market presents several opportunities for growth and innovation:
Market Dynamics
The healthcare fraud analytics market is driven by a combination of internal and external factors. Internal factors include the increasing awareness of healthcare fraud, the need for cost containment, and the desire to improve operational efficiency. External factors include government regulations, advancements in technology, and the evolving healthcare landscape.
The market dynamics of healthcare fraud analytics are influenced by the interplay of these factors. The increasing complexity and volume of healthcare data, coupled with the rising sophistication of fraudulent schemes, necessitate the adoption of advanced analytics solutions. Healthcare organizations are increasingly recognizing the importance of proactive fraud detection and prevention to safeguard their financial resources and maintain the integrity of the healthcare system.
Regional Analysis
The healthcare fraud analytics market exhibits regional variations in terms of adoption and market size. The North American region dominates the market, primarily driven by the presence of established healthcare organizations, advanced data analytics capabilities, and stringent regulations against healthcare fraud. The European market follows closely, with countries like the United Kingdom, Germany, and France investing in fraud detection technologies. The Asia Pacific region is expected to witness significant growth due to the increasing healthcare expenditures, the digital transformation of healthcare systems, and government initiatives to combat fraud.
Competitive Landscape
Leading Companies in the Healthcare Fraud Analytics Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
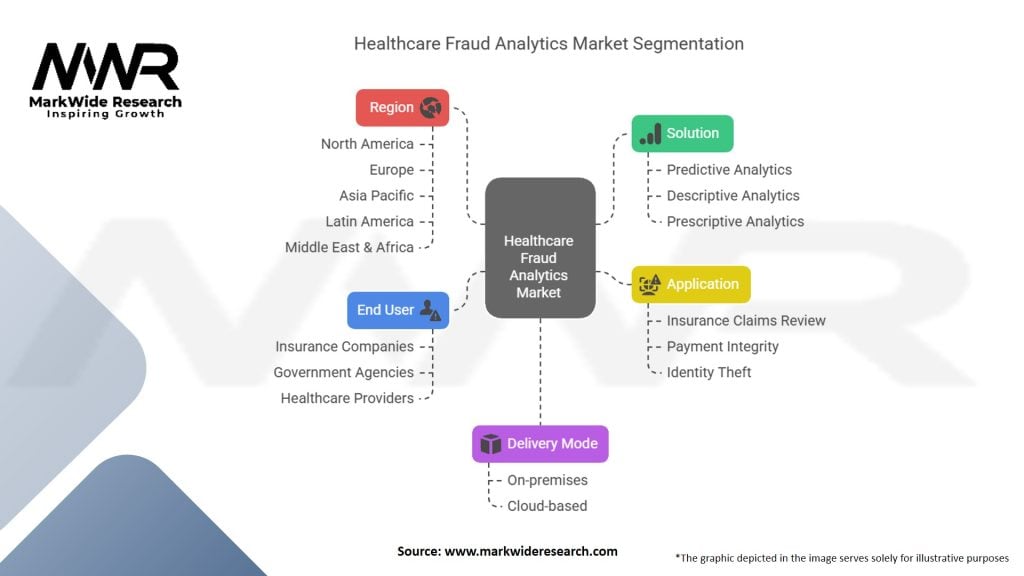
Segmentation
The healthcare fraud analytics market can be segmented based on the type of analytics solutions, deployment models, end-users, and regions. Common types of analytics solutions include predictive analytics, prescriptive analytics, descriptive analytics, and social network analysis. Deployment models can be on-premises, cloud-based, or hybrid. End-users of healthcare fraud analytics solutions include healthcare providers, insurance companies, government agencies, and research institutions.
Category-wise Insights
Key Benefits for Industry Participants and Stakeholders
Industry participants and stakeholders in the healthcare fraud analytics market can derive several key benefits:
SWOT Analysis
A SWOT analysis provides a snapshot of the healthcare fraud analytics market’s strengths, weaknesses, opportunities, and threats:
Strengths:
Weaknesses:
Opportunities:
Threats:
Market Key Trends
Several key trends are shaping the healthcare fraud analytics market:
Covid-19 Impact
The COVID-19 pandemic has had a significant impact on the healthcare industry, including healthcare fraud analytics:
Key Industry Developments
The healthcare fraud analytics market has witnessed several key industry developments:
Analyst Suggestions
Based on market analysis, analysts provide the following suggestions:
Future Outlook
The future of the healthcare fraud analytics market looks promising. Factors such as the increasing prevalence of healthcare fraud, government initiatives to combat fraud, advancements in analytics technologies, and the digital transformation of healthcare systems will continue to drive market growth.
Healthcare organizations will increasingly rely on advanced analytics solutions to detect and prevent fraud, thereby safeguarding their financial resources and ensuring the delivery of quality patient care. The adoption of artificial intelligence, machine learning, and predictive modeling will further enhance the capabilities of fraud analytics systems.
Moreover, the expansion of healthcare fraud analytics into emerging markets and the integration of fraud analytics with electronic health records present significant growth opportunities. However, addressing data privacy and security concerns, overcoming the shortage of skilled professionals, and managing high implementation costs remain key challenges for market growth.
Conclusion
The healthcare fraud analytics market is witnessing rapid growth, driven by the increasing prevalence of healthcare fraud and the adoption of advanced analytics solutions by healthcare organizations. Healthcare fraud analytics enables proactive detection and prevention of fraudulent activities, leading to cost savings and the preservation of financial resources. Technological advancements, government initiatives, and the digitalization of healthcare systems provide opportunities for market growth. However, challenges such as data privacy concerns, the shortage of skilled professionals, and high implementation costs need to be addressed.
What is Healthcare Fraud Analytics?
Healthcare Fraud Analytics refers to the use of data analysis techniques to detect and prevent fraudulent activities within the healthcare system. This includes identifying suspicious billing patterns, analyzing claims data, and monitoring provider behavior to safeguard against financial losses.
What are the key companies in the Healthcare Fraud Analytics Market?
Key companies in the Healthcare Fraud Analytics Market include Optum, IBM Watson Health, SAS Institute, and McKesson Corporation, among others.
What are the main drivers of growth in the Healthcare Fraud Analytics Market?
The main drivers of growth in the Healthcare Fraud Analytics Market include the increasing prevalence of healthcare fraud, the rising costs associated with fraudulent claims, and the growing adoption of advanced analytics technologies to enhance fraud detection capabilities.
What challenges does the Healthcare Fraud Analytics Market face?
Challenges in the Healthcare Fraud Analytics Market include data privacy concerns, the complexity of healthcare regulations, and the need for continuous updates to analytics models to keep pace with evolving fraud tactics.
What opportunities exist in the Healthcare Fraud Analytics Market?
Opportunities in the Healthcare Fraud Analytics Market include the integration of artificial intelligence and machine learning for more accurate fraud detection, the expansion of analytics solutions to smaller healthcare providers, and the potential for collaboration between public and private sectors to enhance fraud prevention efforts.
What trends are shaping the Healthcare Fraud Analytics Market?
Trends shaping the Healthcare Fraud Analytics Market include the increasing use of real-time analytics, the shift towards value-based care models, and the growing emphasis on predictive analytics to proactively identify and mitigate fraud risks.
Healthcare Fraud Analytics Market:
| Segmentation | Details |
|---|---|
| Solution | Predictive Analytics, Descriptive Analytics, Prescriptive Analytics |
| Delivery Mode | On-premises, Cloud-based |
| Application | Insurance Claims Review, Payment Integrity, Identity Theft, Others |
| End User | Insurance Companies, Government Agencies, Healthcare Providers, Others |
| Region | North America, Europe, Asia Pacific, Latin America, Middle East & Africa |
Please note: The segmentation can be entirely customized to align with our client’s needs.
Leading Companies in the Healthcare Fraud Analytics Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
North America
o US
o Canada
o Mexico
Europe
o Germany
o Italy
o France
o UK
o Spain
o Denmark
o Sweden
o Austria
o Belgium
o Finland
o Turkey
o Poland
o Russia
o Greece
o Switzerland
o Netherlands
o Norway
o Portugal
o Rest of Europe
Asia Pacific
o China
o Japan
o India
o South Korea
o Indonesia
o Malaysia
o Kazakhstan
o Taiwan
o Vietnam
o Thailand
o Philippines
o Singapore
o Australia
o New Zealand
o Rest of Asia Pacific
South America
o Brazil
o Argentina
o Colombia
o Chile
o Peru
o Rest of South America
The Middle East & Africa
o Saudi Arabia
o UAE
o Qatar
o South Africa
o Israel
o Kuwait
o Oman
o North Africa
o West Africa
o Rest of MEA
Trusted by Global Leaders
Fortune 500 companies, SMEs, and top institutions rely on MWR’s insights to make informed decisions and drive growth.
ISO & IAF Certified
Our certifications reflect a commitment to accuracy, reliability, and high-quality market intelligence trusted worldwide.
Customized Insights
Every report is tailored to your business, offering actionable recommendations to boost growth and competitiveness.
Multi-Language Support
Final reports are delivered in English and major global languages including French, German, Spanish, Italian, Portuguese, Chinese, Japanese, Korean, Arabic, Russian, and more.
Unlimited User Access
Corporate License offers unrestricted access for your entire organization at no extra cost.
Free Company Inclusion
We add 3–4 extra companies of your choice for more relevant competitive analysis — free of charge.
Post-Sale Assistance
Dedicated account managers provide unlimited support, handling queries and customization even after delivery.
GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at