444 Alaska Avenue
Suite #BAA205 Torrance, CA 90503 USA
+1 424 999 9627
24/7 Customer Support
sales@markwideresearch.com
Email us at
Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at
Corporate User License
Unlimited User Access, Post-Sale Support, Free Updates, Reports in English & Major Languages, and more
$3450
In recent years, the healthcare industry has witnessed significant advancements in technology, transforming various aspects of patient care and administrative operations. One such area is healthcare claims management, where software solutions have revolutionized the way healthcare providers handle claims processing and reimbursement. This comprehensive guide explores the Healthcare Claims Management Software market, providing valuable insights into its meaning, market dynamics, key trends, regional analysis, competitive landscape, and future outlook.
Healthcare Claims Management Software refers to specialized software solutions designed to automate and streamline the claims processing workflow in healthcare organizations. These systems enable efficient management of claims from submission to reimbursement, reducing manual errors, improving accuracy, and accelerating the overall claims processing cycle.
Executive Summary:
The Healthcare Claims Management Software market is witnessing significant growth due to the increasing adoption of electronic health records (EHR), the need for cost containment, and the rising complexities of the healthcare reimbursement process. This executive summary provides a concise overview of the market’s key highlights, including market drivers, restraints, opportunities, and key industry developments.
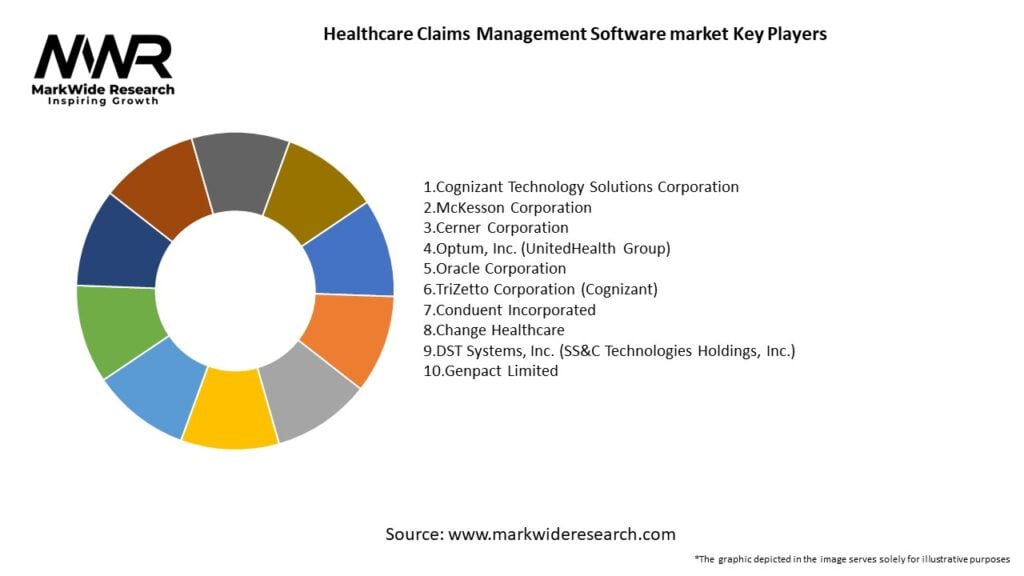
Important Note: The companies listed in the image above are for reference only. The final study will cover 18–20 key players in this market, and the list can be adjusted based on our client’s requirements.
Key Market Insights:
Market Drivers:
Market Restraints:
Market Opportunities:

Market Dynamics:
The Healthcare Claims Management Software market is characterized by intense competition and continuous technological advancements. Key market dynamics include evolving regulations, shifting consumer expectations, strategic partnerships, mergers and acquisitions, and the emergence of niche players focusing on specific segments within the claims management process.
Regional Analysis:
Competitive Landscape:
Leading Companies in the Healthcare Claims Management Software Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.

Segmentation:
The Healthcare Claims Management Software market can be segmented based on deployment type (cloud-based and on-premises), end-user (hospitals, clinics, and other healthcare providers), and region.
Category-wise Insights:
Key Benefits for Industry Participants and Stakeholders:
SWOT Analysis:
Market Key Trends:
Covid-19 Impact:
The COVID-19 pandemic has accelerated the adoption of telehealth services and remote claims processing solutions. Healthcare organizations faced unprecedented challenges in managing claims during the pandemic, leading to increased demand for efficient claims management software.
Key Industry Developments:
Analyst Suggestions:
Future Outlook:
The Healthcare Claims Management Software market is poised for significant growth in the coming years. Technological advancements, increasing digitization of healthcare systems, and the need for efficient claims processing are driving market expansion. The integration of AI, ML, and blockchain technologies, along with the rising demand for telehealth services, will shape the future of the market.
Conclusion:
The Healthcare Claims Management Software market presents lucrative opportunities for software vendors and healthcare organizations alike. By leveraging advanced technology solutions, healthcare providers can streamline their claims processing operations, enhance revenue cycles, and improve patient care. With continuous innovation and a customer-centric approach, stakeholders in the market can navigate the evolving landscape and achieve long-term success.
What is Healthcare Claims Management Software?
Healthcare Claims Management Software refers to systems designed to streamline the processing of healthcare claims, ensuring accurate billing and reimbursement. These solutions help healthcare providers manage claims submissions, track payment statuses, and reduce errors in billing.
What are the key players in the Healthcare Claims Management Software market?
Key players in the Healthcare Claims Management Software market include companies like Optum, Change Healthcare, and McKesson, which provide comprehensive solutions for claims processing and management, among others.
What are the main drivers of growth in the Healthcare Claims Management Software market?
The growth of the Healthcare Claims Management Software market is driven by the increasing need for efficient claims processing, the rise in healthcare expenditures, and the demand for improved patient care through accurate billing practices.
What challenges does the Healthcare Claims Management Software market face?
Challenges in the Healthcare Claims Management Software market include the complexity of healthcare regulations, the need for interoperability between different systems, and the potential for data security breaches.
What opportunities exist in the Healthcare Claims Management Software market?
Opportunities in the Healthcare Claims Management Software market include the integration of artificial intelligence for better claims processing, the expansion of telehealth services, and the growing emphasis on value-based care models.
What trends are shaping the Healthcare Claims Management Software market?
Trends in the Healthcare Claims Management Software market include the adoption of cloud-based solutions, the use of analytics for decision-making, and the increasing focus on patient-centric billing practices.
Healthcare Claims Management Software market
| Segmentation Details | Description |
|---|---|
| Product Type | Claims Processing, Billing Management, Fraud Detection, Analytics Tools |
| End User | Insurance Providers, Healthcare Payers, Third-Party Administrators, Self-Insured Employers |
| Deployment | On-Premises, Cloud-Based, Hybrid, SaaS |
| Solution | Integrated Solutions, Standalone Applications, Custom Solutions, Others |
Please note: The segmentation can be entirely customized to align with our client’s needs.
Leading Companies in the Healthcare Claims Management Software Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
North America
o US
o Canada
o Mexico
Europe
o Germany
o Italy
o France
o UK
o Spain
o Denmark
o Sweden
o Austria
o Belgium
o Finland
o Turkey
o Poland
o Russia
o Greece
o Switzerland
o Netherlands
o Norway
o Portugal
o Rest of Europe
Asia Pacific
o China
o Japan
o India
o South Korea
o Indonesia
o Malaysia
o Kazakhstan
o Taiwan
o Vietnam
o Thailand
o Philippines
o Singapore
o Australia
o New Zealand
o Rest of Asia Pacific
South America
o Brazil
o Argentina
o Colombia
o Chile
o Peru
o Rest of South America
The Middle East & Africa
o Saudi Arabia
o UAE
o Qatar
o South Africa
o Israel
o Kuwait
o Oman
o North Africa
o West Africa
o Rest of MEA
Trusted by Global Leaders
Fortune 500 companies, SMEs, and top institutions rely on MWR’s insights to make informed decisions and drive growth.
ISO & IAF Certified
Our certifications reflect a commitment to accuracy, reliability, and high-quality market intelligence trusted worldwide.
Customized Insights
Every report is tailored to your business, offering actionable recommendations to boost growth and competitiveness.
Multi-Language Support
Final reports are delivered in English and major global languages including French, German, Spanish, Italian, Portuguese, Chinese, Japanese, Korean, Arabic, Russian, and more.
Unlimited User Access
Corporate License offers unrestricted access for your entire organization at no extra cost.
Free Company Inclusion
We add 3–4 extra companies of your choice for more relevant competitive analysis — free of charge.
Post-Sale Assistance
Dedicated account managers provide unlimited support, handling queries and customization even after delivery.
GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at