444 Alaska Avenue
Suite #BAA205 Torrance, CA 90503 USA
+1 424 999 9627
24/7 Customer Support
sales@markwideresearch.com
Email us at
Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at
Corporate User License
Unlimited User Access, Post-Sale Support, Free Updates, Reports in English & Major Languages, and more
$3450
Market Overview
The Global Healthcare Payers Core Administrative Processing Solutions Software market refers to the market for software solutions that cater to the core administrative processing needs of healthcare payers. These solutions are designed to streamline and automate various tasks related to claims processing, enrollment, billing, and other administrative functions in the healthcare insurance industry.
Meaning
Healthcare payers, such as insurance companies, face numerous challenges in managing their administrative processes efficiently. The use of core administrative processing solutions software helps them overcome these challenges by providing a centralized platform for managing and automating various tasks. This software enables payers to handle large volumes of data, improve accuracy, reduce operational costs, and enhance overall efficiency.
Executive Summary
The Global Healthcare Payers Core Administrative Processing Solutions Software market is witnessing significant growth due to the increasing need for efficient and streamlined administrative processes in the healthcare insurance industry. Payers are increasingly adopting software solutions to automate their core administrative functions and improve overall operational efficiency. The market is characterized by intense competition among key players who offer a wide range of solutions to cater to the diverse needs of healthcare payers.
Important Note: The companies listed in the image above are for reference only. The final study will cover 18–20 key players in this market, and the list can be adjusted based on our client’s requirements.
Key Market Insights
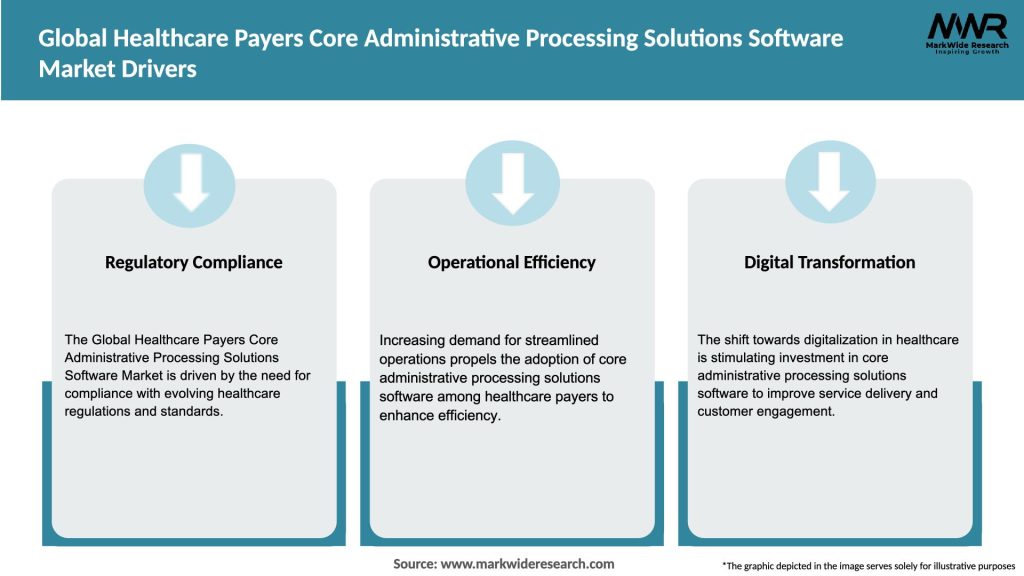
Market Drivers
Market Restraints
Market Opportunities

Market Dynamics
The Global Healthcare Payers Core Administrative Processing Solutions Software market is dynamic and influenced by various factors. Technological advancements, changing regulatory landscapes, market competition, and evolving customer expectations all play a significant role in shaping the market dynamics. Payers are continuously seeking solutions that offer greater automation, improved data analytics capabilities, and enhanced security features.
Regional Analysis
The market for Healthcare Payers Core Administrative Processing Solutions Software is geographically diverse, with key regions including North America, Europe, Asia Pacific, Latin America, and the Middle East and Africa. North America dominates the market due to the presence of major healthcare insurance players and advanced healthcare infrastructure. However, the Asia Pacific region is expected to witness rapid growth, driven by the increasing adoption of healthcare insurance and digital transformation initiatives in the healthcare sector.
Competitive Landscape
Leading Companies in the Global Healthcare Payers Core Administrative Processing Solutions Software Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
Segmentation
The market for Healthcare Payers Core Administrative Processing Solutions Software can be segmented based on various factors, including deployment type, end-user, and application. Deployment types may include on-premises, cloud-based, and hybrid solutions. End-users can be categorized as insurance companies, third-party administrators, and government agencies. Applications may cover claims processing, enrollment and eligibility management, billing and payments, provider network management, and customer relationship management.
Category-wise Insights
Key Benefits for Industry Participants and Stakeholders
SWOT Analysis
Strengths:
Weaknesses:
Opportunities:
Threats:
Market Key Trends
Covid-19 Impact
The COVID-19 pandemic had a significant impact on the healthcare industry, including healthcare payers and their administrative processes. The need for remote work capabilities, increased reliance on digital solutions, and the urgency to manage claims and payments efficiently created a demand for core administrative processing solutions software. Payers accelerated their digital transformation efforts and adopted software solutions to overcome operational challenges caused by the pandemic.
Key Industry Developments
Analyst Suggestions
Future Outlook
The future outlook for the Global Healthcare Payers Core Administrative Processing Solutions Software market is promising. The market is expected to witness steady growth as healthcare payers continue to prioritize operational efficiency, cost reduction, and improved customer experiences. Technological advancements, such as AI, ML, and cloud computing, will continue to drive innovation in the market. The integration of blockchain, the expansion of telehealth services, and interoperability with EHR systems will further shape the future of core administrative processing solutions software.
Conclusion
The Global Healthcare Payers Core Administrative Processing Solutions Software market is experiencing significant growth driven by the need for streamlined administrative processes in the healthcare insurance industry. The market offers opportunities for automation, cost reduction, and data-driven insights through advanced software solutions. Despite implementation challenges and security concerns, the market is expected to expand, fueled by technological advancements, emerging markets, and collaborations. Healthcare payers and industry stakeholders should embrace digital transformation, focus on user experience, and prioritize data analytics to stay competitive and meet evolving market demands.
What is Healthcare Payers Core Administrative Processing Solutions Software?
Healthcare Payers Core Administrative Processing Solutions Software refers to systems designed to streamline administrative tasks for healthcare payers, including claims processing, billing, and member management. These solutions enhance operational efficiency and improve service delivery in the healthcare sector.
What are the key players in the Global Healthcare Payers Core Administrative Processing Solutions Software Market?
Key players in the Global Healthcare Payers Core Administrative Processing Solutions Software Market include companies like Optum, Cognizant, and McKesson, which provide comprehensive solutions for healthcare administration. These companies focus on improving efficiency and compliance in healthcare operations, among others.
What are the growth factors driving the Global Healthcare Payers Core Administrative Processing Solutions Software Market?
The growth of the Global Healthcare Payers Core Administrative Processing Solutions Software Market is driven by the increasing demand for efficient claims processing, the need for regulatory compliance, and the rising adoption of digital health solutions. Additionally, the shift towards value-based care is propelling the need for advanced administrative tools.
What challenges does the Global Healthcare Payers Core Administrative Processing Solutions Software Market face?
Challenges in the Global Healthcare Payers Core Administrative Processing Solutions Software Market include data security concerns, the complexity of integrating new solutions with existing systems, and the need for continuous updates to comply with changing regulations. These factors can hinder the adoption of new technologies.
What opportunities exist in the Global Healthcare Payers Core Administrative Processing Solutions Software Market?
Opportunities in the Global Healthcare Payers Core Administrative Processing Solutions Software Market include the potential for innovation in artificial intelligence and machine learning applications, which can enhance data analytics and decision-making processes. Additionally, the growing trend of telehealth services presents new avenues for administrative solutions.
What trends are shaping the Global Healthcare Payers Core Administrative Processing Solutions Software Market?
Trends shaping the Global Healthcare Payers Core Administrative Processing Solutions Software Market include the increasing use of cloud-based solutions, the integration of advanced analytics for better decision-making, and a focus on user-friendly interfaces to improve the user experience. These trends are driving the evolution of administrative processing in healthcare.
Global Healthcare Payers Core Administrative Processing Solutions Software Market
| Segmentation Details | Description |
|---|---|
| Product Type | Claims Management, Billing Solutions, Enrollment Management, Payment Processing |
| End User | Insurance Providers, Third-Party Administrators, Healthcare Organizations, Government Programs |
| Deployment | On-Premises, Cloud-Based, Hybrid, SaaS |
| Service Type | Consulting, Implementation, Support, Maintenance |
Please note: The segmentation can be entirely customized to align with our client’s needs.
Leading Companies in the Global Healthcare Payers Core Administrative Processing Solutions Software Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
North America
o US
o Canada
o Mexico
Europe
o Germany
o Italy
o France
o UK
o Spain
o Denmark
o Sweden
o Austria
o Belgium
o Finland
o Turkey
o Poland
o Russia
o Greece
o Switzerland
o Netherlands
o Norway
o Portugal
o Rest of Europe
Asia Pacific
o China
o Japan
o India
o South Korea
o Indonesia
o Malaysia
o Kazakhstan
o Taiwan
o Vietnam
o Thailand
o Philippines
o Singapore
o Australia
o New Zealand
o Rest of Asia Pacific
South America
o Brazil
o Argentina
o Colombia
o Chile
o Peru
o Rest of South America
The Middle East & Africa
o Saudi Arabia
o UAE
o Qatar
o South Africa
o Israel
o Kuwait
o Oman
o North Africa
o West Africa
o Rest of MEA
Trusted by Global Leaders
Fortune 500 companies, SMEs, and top institutions rely on MWR’s insights to make informed decisions and drive growth.
ISO & IAF Certified
Our certifications reflect a commitment to accuracy, reliability, and high-quality market intelligence trusted worldwide.
Customized Insights
Every report is tailored to your business, offering actionable recommendations to boost growth and competitiveness.
Multi-Language Support
Final reports are delivered in English and major global languages including French, German, Spanish, Italian, Portuguese, Chinese, Japanese, Korean, Arabic, Russian, and more.
Unlimited User Access
Corporate License offers unrestricted access for your entire organization at no extra cost.
Free Company Inclusion
We add 3–4 extra companies of your choice for more relevant competitive analysis — free of charge.
Post-Sale Assistance
Dedicated account managers provide unlimited support, handling queries and customization even after delivery.
GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at