444 Alaska Avenue
Suite #BAA205 Torrance, CA 90503 USA
+1 424 999 9627
24/7 Customer Support
sales@markwideresearch.com
Email us at
Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at
Corporate User License
Unlimited User Access, Post-Sale Support, Free Updates, Reports in English & Major Languages, and more
$2450
Market Overview
The post-traumatic stress disorder (PTSD) treatment market in Australia is a critical component of the nation’s mental health landscape, addressing the needs of individuals who have experienced traumatic events. PTSD, characterized by intrusive memories, hyperarousal, and avoidance behaviors, requires specialized interventions to promote healing and recovery. Australia’s healthcare system offers a range of therapeutic modalities and support services to address the unique needs of individuals living with PTSD.
Meaning
PTSD treatment in Australia encompasses a variety of approaches aimed at reducing symptoms, improving coping strategies, and enhancing overall well-being. This may include evidence-based psychotherapies, pharmacotherapy, alternative therapies, and peer support programs. Treatment providers collaborate across disciplines to deliver comprehensive care tailored to individual needs and preferences.
Executive Summary
The PTSD treatment market in Australia is experiencing significant growth, driven by increased awareness, expanding mental health infrastructure, and advancements in evidence-based practices. While the market presents opportunities for providers to innovate and improve care delivery, challenges such as stigma, treatment accessibility barriers, and workforce shortages persist. Addressing these challenges requires a concerted effort from stakeholders across sectors.

Important Note: The companies listed in the image above are for reference only. The final study will cover 18–20 key players in this market, and the list can be adjusted based on our client’s requirements.
Key Market Insights
Market Drivers
Market Restraints
Market Opportunities
Market Dynamics
The PTSD treatment market in Australia operates within a dynamic landscape shaped by socio-cultural factors, policy changes, technological advancements, and healthcare system reforms. Market dynamics influence service delivery models, provider-patient interactions, treatment outcomes, and public health priorities, highlighting the importance of adaptability and innovation in addressing evolving needs.
Regional Analysis
The distribution of PTSD treatment services in Australia varies across regions, influenced by population density, healthcare infrastructure, and socioeconomic factors. Urban centers may have greater access to specialized mental health providers, academic medical centers, and research institutions, while rural and remote areas may face challenges in service availability and workforce capacity. Targeted interventions are needed to address regional disparities and improve access to care for all individuals affected by PTSD.
Competitive Landscape
Leading Companies in Australia Post-Traumatic Stress Disorder Treatment Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
Segmentation
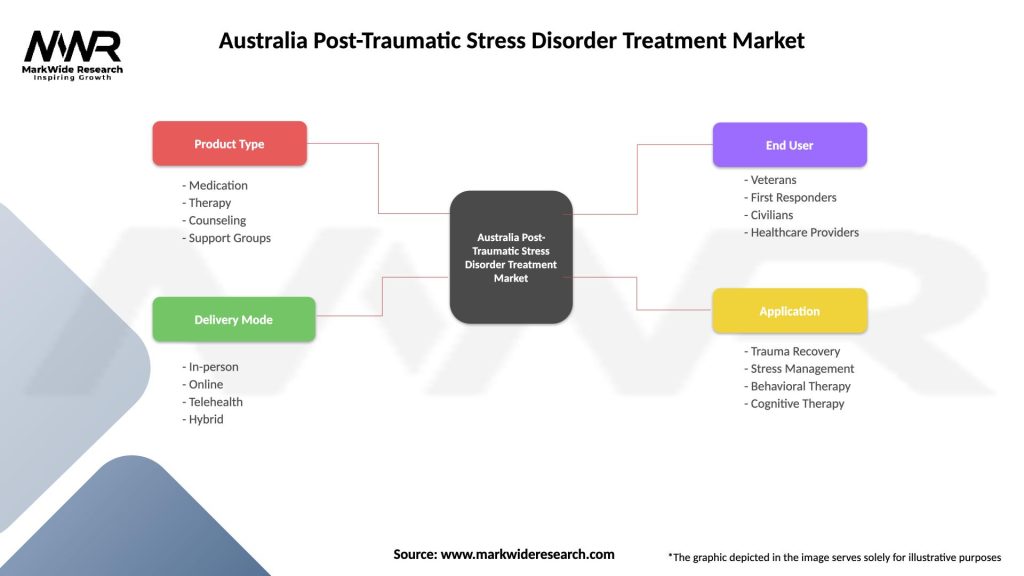
The PTSD treatment market in Australia can be segmented based on various factors, including:
Segmentation enables a nuanced understanding of market dynamics and patient needs, guiding service planning, resource allocation, and intervention strategies.
Category-wise Insights
Key Benefits for Industry Participants and Stakeholders
SWOT Analysis
Understanding these factors through a SWOT analysis helps businesses identify their competitive advantages, address weaknesses, capitalize on opportunities, and mitigate potential threats.
Market Key Trends
Covid-19 Impact
The COVID-19 pandemic has had a significant impact on PTSD treatment in Australia, exacerbating existing challenges while highlighting opportunities for innovation and adaptation. The pandemic has increased demand for mental health services, disrupted care delivery, and heightened stress and trauma levels in the population. Telehealth adoption, community resilience initiatives, and trauma-informed responses have emerged as key strategies to address the pandemic’s mental health implications and support individuals living with PTSD.
Key Industry Developments
Analyst Suggestions
Future Outlook
The PTSD treatment market in Australia is poised for continued growth and evolution, driven by increasing demand for mental healthcare services, technological advancements, and shifting societal attitudes toward mental illness. Addressing treatment accessibility barriers, promoting early intervention strategies, and fostering collaboration across sectors will be critical to advancing PTSD care and improving outcomes for individuals affected by trauma.
Conclusion
The PTSD treatment market in Australia plays a vital role in addressing the mental health needs of individuals affected by trauma. While the market presents significant opportunities for providers to innovate and expand service delivery, challenges such as stigma, treatment accessibility barriers, and workforce shortages persist. By embracing evidence-based practices, leveraging technological advancements, and fostering collaboration across sectors, stakeholders can enhance PTSD care delivery, promote resilience, and support recovery for individuals living with trauma-related disorders.
What is Post-Traumatic Stress Disorder Treatment?
Post-Traumatic Stress Disorder Treatment refers to the various therapeutic approaches and interventions designed to help individuals suffering from PTSD manage their symptoms and improve their quality of life. This can include psychotherapy, medication, and support groups, among other methods.
What are the key players in the Australia Post-Traumatic Stress Disorder Treatment Market?
Key players in the Australia Post-Traumatic Stress Disorder Treatment Market include organizations such as Beyond Blue, the Australian Centre for Posttraumatic Mental Health, and various private mental health clinics, among others.
What are the main drivers of growth in the Australia Post-Traumatic Stress Disorder Treatment Market?
The growth of the Australia Post-Traumatic Stress Disorder Treatment Market is driven by increasing awareness of mental health issues, a rise in PTSD cases due to various factors such as trauma from natural disasters and military service, and advancements in treatment methodologies.
What challenges does the Australia Post-Traumatic Stress Disorder Treatment Market face?
Challenges in the Australia Post-Traumatic Stress Disorder Treatment Market include stigma surrounding mental health, limited access to specialized care in rural areas, and the variability in treatment effectiveness among individuals.
What opportunities exist in the Australia Post-Traumatic Stress Disorder Treatment Market?
Opportunities in the Australia Post-Traumatic Stress Disorder Treatment Market include the development of innovative therapies, increased funding for mental health services, and the potential for telehealth solutions to reach underserved populations.
What trends are shaping the Australia Post-Traumatic Stress Disorder Treatment Market?
Trends in the Australia Post-Traumatic Stress Disorder Treatment Market include a growing emphasis on personalized treatment plans, the integration of technology in therapy, and a focus on holistic approaches that address both mental and physical health.
Australia Post-Traumatic Stress Disorder Treatment Market
| Segmentation Details | Description |
|---|---|
| Product Type | Medication, Therapy, Counseling, Support Groups |
| Delivery Mode | In-person, Online, Telehealth, Hybrid |
| End User | Veterans, First Responders, Civilians, Healthcare Providers |
| Application | Trauma Recovery, Stress Management, Behavioral Therapy, Cognitive Therapy |
Please note: The segmentation can be entirely customized to align with our client’s needs.
Leading Companies in Australia Post-Traumatic Stress Disorder Treatment Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
Trusted by Global Leaders
Fortune 500 companies, SMEs, and top institutions rely on MWR’s insights to make informed decisions and drive growth.
ISO & IAF Certified
Our certifications reflect a commitment to accuracy, reliability, and high-quality market intelligence trusted worldwide.
Customized Insights
Every report is tailored to your business, offering actionable recommendations to boost growth and competitiveness.
Multi-Language Support
Final reports are delivered in English and major global languages including French, German, Spanish, Italian, Portuguese, Chinese, Japanese, Korean, Arabic, Russian, and more.
Unlimited User Access
Corporate License offers unrestricted access for your entire organization at no extra cost.
Free Company Inclusion
We add 3–4 extra companies of your choice for more relevant competitive analysis — free of charge.
Post-Sale Assistance
Dedicated account managers provide unlimited support, handling queries and customization even after delivery.
GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at