444 Alaska Avenue
Suite #BAA205 Torrance, CA 90503 USA
+1 424 999 9627
24/7 Customer Support
sales@markwideresearch.com
Email us at
Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at

Corporate User License
Unlimited User Access, Post-Sale Support, Free Updates, Reports in English & Major Languages, and more
$3450
The AI in medical billing market represents a transformative segment within healthcare technology, revolutionizing how medical practices, hospitals, and healthcare systems manage their revenue cycle operations. This rapidly expanding market encompasses artificial intelligence solutions designed to automate, streamline, and optimize medical billing processes, from patient registration and insurance verification to claims processing and payment collection. Healthcare organizations are increasingly adopting AI-powered billing solutions to address persistent challenges including claim denials, coding errors, and administrative inefficiencies that have plagued the industry for decades.
Market dynamics indicate robust growth driven by the increasing complexity of healthcare regulations, rising healthcare costs, and the urgent need for operational efficiency. The integration of machine learning algorithms, natural language processing, and predictive analytics into medical billing workflows is enabling healthcare providers to achieve significant improvements in accuracy, speed, and cost-effectiveness. AI technologies are particularly effective in automating repetitive tasks such as data entry, code assignment, and claim status tracking, allowing healthcare professionals to focus on patient care rather than administrative burdens.
Regional adoption patterns show North America leading the market due to advanced healthcare infrastructure, stringent regulatory requirements, and high healthcare spending. The market is experiencing accelerated growth at a CAGR of approximately 12.8%, with increasing penetration across various healthcare settings including hospitals, clinics, and ambulatory surgical centers. Technology advancement continues to drive innovation, with emerging capabilities in real-time claim processing, automated denial management, and intelligent revenue optimization becoming standard features in modern AI billing solutions.
The AI in medical billing market refers to the comprehensive ecosystem of artificial intelligence technologies, software solutions, and services specifically designed to automate and optimize healthcare revenue cycle management processes. This market encompasses various AI-powered tools that assist healthcare organizations in managing patient billing, insurance claims processing, payment collection, and financial reporting through intelligent automation and data analysis.
Core components of this market include machine learning algorithms for predictive analytics, natural language processing for automated coding, robotic process automation for repetitive tasks, and intelligent workflow management systems. These technologies work collectively to reduce manual intervention, minimize errors, and accelerate the entire billing cycle from patient encounter to payment receipt. AI solutions in medical billing typically integrate with existing electronic health records (EHR) systems, practice management software, and healthcare information systems to create seamless, automated workflows.
Market participants include software vendors developing AI billing solutions, healthcare technology companies offering integrated platforms, consulting firms providing implementation services, and healthcare organizations adopting these technologies. The market serves various end-users including hospitals, physician practices, ambulatory surgical centers, and third-party billing companies seeking to improve operational efficiency and financial performance through intelligent automation.
Strategic market analysis reveals that the AI in medical billing market is experiencing unprecedented growth driven by the healthcare industry’s digital transformation initiatives and the pressing need for operational efficiency. Healthcare organizations are increasingly recognizing the potential of artificial intelligence to address longstanding challenges in revenue cycle management, including high claim denial rates, coding errors, and administrative costs that can consume up to 30% of healthcare revenue.
Technology adoption is accelerating across all healthcare segments, with large hospital systems leading the implementation of comprehensive AI billing solutions, while smaller practices are adopting targeted AI tools for specific billing functions. The market is characterized by rapid innovation, with vendors continuously enhancing their offerings through advanced machine learning capabilities, improved integration features, and expanded functionality covering the entire revenue cycle spectrum.
Competitive landscape shows a mix of established healthcare technology companies and emerging AI specialists competing to capture market share through differentiated solutions and strategic partnerships. Key market drivers include regulatory compliance requirements, value-based care initiatives, and the growing emphasis on patient financial experience. Market challenges primarily revolve around data security concerns, integration complexities, and the need for staff training to effectively utilize AI-powered billing systems.
Future projections indicate continued robust growth as healthcare organizations recognize the measurable return on investment from AI billing implementations, with early adopters reporting significant improvements in claim acceptance rates, reduced processing times, and enhanced cash flow management.
Market intelligence reveals several critical insights that are shaping the AI in medical billing landscape and driving strategic decision-making among healthcare organizations and technology vendors:
Primary market drivers propelling the growth of AI in medical billing include the increasing complexity of healthcare reimbursement systems and the urgent need for operational efficiency in healthcare organizations facing mounting financial pressures. The transition to value-based care models has created additional complexity in billing and reimbursement processes, making AI solutions essential for managing multiple payment methodologies and quality metrics.
Regulatory compliance requirements continue to drive adoption as healthcare organizations must navigate constantly evolving billing regulations, coding updates, and payer requirements. AI systems provide automated compliance monitoring and real-time updates, reducing the risk of costly penalties and claim denials. The implementation of ICD-10 coding systems and other complex medical coding standards has increased the demand for intelligent automation that can accurately assign codes and identify potential compliance issues.
Financial pressures on healthcare organizations, including reduced reimbursement rates and increased patient financial responsibility, are compelling providers to optimize their revenue cycle operations. AI billing solutions offer measurable improvements in cash flow, reduced days in accounts receivable, and enhanced collection rates. Labor shortages in healthcare administration, particularly in medical coding and billing roles, are driving organizations to seek AI-powered alternatives that can maintain productivity while reducing dependence on specialized human resources.
Technology advancement in machine learning, natural language processing, and cloud computing has made AI billing solutions more accessible, affordable, and effective than ever before. The increasing availability of healthcare data and improved interoperability standards enable AI systems to deliver more accurate and comprehensive billing automation across diverse healthcare environments.
Implementation challenges represent significant restraints in the AI medical billing market, particularly for smaller healthcare organizations with limited IT resources and technical expertise. The complexity of integrating AI solutions with existing healthcare information systems often requires substantial time, effort, and specialized knowledge that may not be readily available within healthcare organizations. Data quality issues can also impede successful AI implementation, as these systems require clean, standardized data to function effectively.
Security and privacy concerns remain paramount in healthcare, where patient data protection is both a regulatory requirement and ethical obligation. Healthcare organizations are cautious about adopting AI solutions that may introduce new security vulnerabilities or compliance risks. The need for robust cybersecurity measures and comprehensive data governance frameworks can slow adoption and increase implementation costs.
Cost considerations pose challenges for many healthcare organizations, particularly smaller practices operating with tight budgets. While AI billing solutions offer long-term cost savings, the initial investment in software, implementation, training, and ongoing maintenance can be substantial. Return on investment timelines may extend beyond what some organizations can comfortably manage, especially when facing immediate financial pressures.
Resistance to change within healthcare organizations can slow adoption, as staff members may be hesitant to embrace new technologies that alter established workflows. The need for comprehensive training and change management initiatives adds complexity and cost to AI billing implementations. Regulatory uncertainty regarding AI use in healthcare billing and the potential for changing compliance requirements can also create hesitation among healthcare decision-makers.
Emerging opportunities in the AI medical billing market are substantial, driven by the healthcare industry’s ongoing digital transformation and the increasing recognition of AI’s potential to solve complex operational challenges. The expansion of telehealth services and remote patient care has created new billing scenarios that require sophisticated AI solutions to manage diverse service delivery models and associated reimbursement complexities.
Small and medium healthcare practices represent a significant untapped market opportunity, as many have yet to fully embrace AI billing technologies due to cost and complexity concerns. The development of more affordable, user-friendly AI solutions specifically designed for smaller practices could unlock substantial market growth. Cloud-based AI platforms are making advanced billing automation more accessible to organizations of all sizes through subscription-based models that reduce upfront investment requirements.
International expansion presents considerable opportunities as healthcare systems worldwide seek to modernize their billing and revenue cycle operations. Emerging markets with developing healthcare infrastructure are particularly attractive for AI billing solution providers. Specialized healthcare sectors including mental health, dental care, and veterinary services offer niche opportunities for tailored AI billing solutions that address sector-specific requirements and regulations.
Integration opportunities with emerging healthcare technologies such as blockchain for secure transactions, IoT devices for automated data collection, and advanced analytics for population health management could create new market segments and revenue streams. The growing emphasis on patient financial experience opens opportunities for AI solutions that enhance billing transparency, payment options, and customer service automation.
Market dynamics in the AI medical billing sector are characterized by rapid technological evolution, shifting healthcare regulations, and changing payer requirements that continuously reshape the competitive landscape. The interplay between healthcare providers seeking operational efficiency and technology vendors developing increasingly sophisticated AI solutions creates a dynamic environment where innovation drives market growth and differentiation.
Competitive pressures are intensifying as established healthcare technology companies expand their AI capabilities while new entrants bring specialized AI expertise to the market. This competition is driving rapid innovation cycles, with vendors regularly introducing enhanced features, improved accuracy, and expanded functionality to maintain market position. Strategic partnerships between AI technology companies and healthcare organizations are becoming increasingly common, enabling collaborative development of solutions that address specific market needs.
Regulatory evolution continues to influence market dynamics as healthcare authorities develop guidelines for AI use in healthcare operations. These regulatory developments create both opportunities and challenges, requiring vendors to maintain compliance while pursuing innovation. Payer requirements are also evolving, with insurance companies increasingly demanding electronic transactions and automated processing capabilities that favor AI-enabled billing systems.
Technology convergence is creating new market dynamics as AI billing solutions integrate with other healthcare technologies including electronic health records, practice management systems, and patient engagement platforms. This convergence is leading to more comprehensive, integrated solutions that offer greater value to healthcare organizations. Data analytics capabilities are becoming increasingly important, with organizations seeking AI solutions that provide actionable insights for revenue optimization and operational improvement, achieving efficiency gains of up to 40% in billing operations.
Comprehensive research methodology employed in analyzing the AI in medical billing market encompasses both primary and secondary research approaches to ensure accurate, reliable, and actionable market intelligence. The research framework combines quantitative data analysis with qualitative insights from industry experts, healthcare professionals, and technology vendors to provide a holistic view of market dynamics and trends.
Primary research activities include structured interviews with healthcare executives, billing managers, and IT professionals across various healthcare settings to understand adoption patterns, implementation challenges, and success factors. Surveys conducted among healthcare organizations provide quantitative insights into market penetration, technology preferences, and investment priorities. Expert consultations with AI technology specialists and healthcare industry analysts contribute valuable perspectives on technological capabilities and market evolution.
Secondary research methodology involves comprehensive analysis of industry reports, regulatory documents, company financial statements, and technology publications to identify market trends, competitive positioning, and growth drivers. Patent analysis and technology assessment provide insights into innovation trends and emerging capabilities in AI billing solutions. Market data validation processes ensure accuracy and reliability through cross-referencing multiple sources and expert verification.
Analytical frameworks employed include market sizing models, competitive analysis matrices, and trend projection methodologies that account for various market variables and scenarios. The research methodology incorporates both bottom-up and top-down approaches to market analysis, ensuring comprehensive coverage of all market segments and stakeholder perspectives. Continuous monitoring of market developments and regular updates to research findings ensure the analysis remains current and relevant to market participants.
North American market dominates the AI in medical billing landscape, accounting for approximately 65% of global market share, driven by advanced healthcare infrastructure, stringent regulatory requirements, and high adoption rates of healthcare technology. The United States leads regional growth with widespread implementation across large hospital systems and integrated delivery networks. Regulatory frameworks including HIPAA compliance and Medicare requirements have accelerated AI adoption as organizations seek automated solutions to manage complex compliance obligations.
European markets demonstrate strong growth potential, particularly in countries with nationalized healthcare systems seeking to optimize operational efficiency and cost management. The United Kingdom, Germany, and France are leading European adoption, with GDPR compliance requirements driving demand for AI solutions that incorporate robust data protection capabilities. European healthcare organizations are particularly focused on AI solutions that support value-based care initiatives and population health management.
Asia-Pacific region represents the fastest-growing market segment, with countries like Japan, Australia, and Singapore investing heavily in healthcare digitization initiatives. The region’s growth is fueled by aging populations, increasing healthcare spending, and government initiatives promoting healthcare technology adoption. Emerging markets in Asia-Pacific are leapfrogging traditional billing systems to implement AI-powered solutions directly.
Latin American and Middle Eastern markets show promising growth trajectories as healthcare systems modernize and seek to improve operational efficiency. These regions present opportunities for AI billing vendors to establish early market presence and develop solutions tailored to local regulatory and operational requirements. Market penetration in these regions is expected to accelerate as cloud-based AI solutions become more accessible and affordable for healthcare organizations with varying technology budgets.
Competitive dynamics in the AI medical billing market feature a diverse ecosystem of established healthcare technology companies, specialized AI vendors, and emerging startups competing across various market segments and customer types. The landscape is characterized by rapid innovation, strategic partnerships, and continuous product enhancement as companies seek to differentiate their offerings and capture market share.
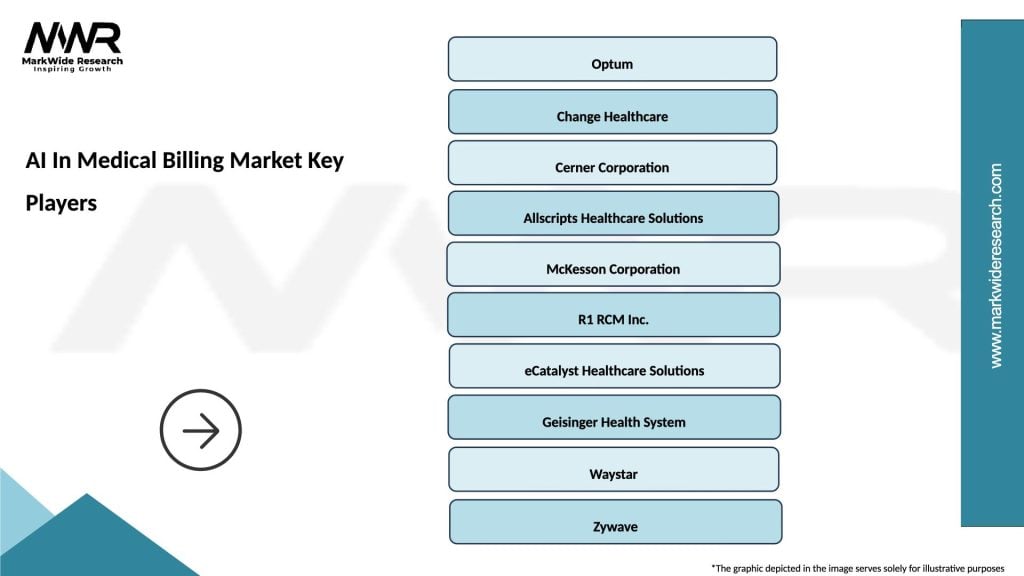
Market leaders include established healthcare technology companies that have integrated AI capabilities into their existing billing and revenue cycle management platforms:
Specialized AI vendors are also gaining market traction by focusing exclusively on artificial intelligence solutions for healthcare billing, offering innovative approaches and advanced capabilities that complement or compete with traditional healthcare technology providers. These companies often provide more sophisticated AI algorithms and specialized functionality for specific billing challenges.
Strategic partnerships between AI technology companies and healthcare organizations are becoming increasingly common, enabling collaborative development of customized solutions and accelerating market adoption through proven use cases and success stories.
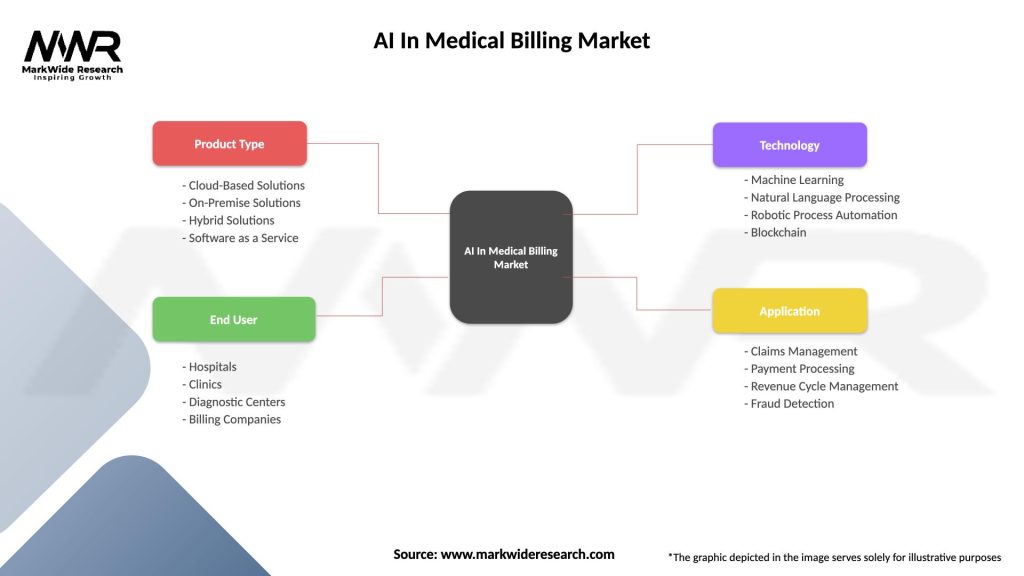
Market segmentation analysis reveals distinct categories within the AI medical billing market, each serving specific customer needs and operational requirements. Understanding these segments is crucial for vendors developing targeted solutions and healthcare organizations evaluating technology options.
By Technology Type:
By Application Area:
By End User:
Hospital and health system segment represents the largest market category, driven by complex billing requirements, high transaction volumes, and substantial resources available for technology investment. These organizations typically implement comprehensive AI billing platforms that integrate with existing EHR systems and provide enterprise-wide automation capabilities. Large hospital systems are achieving significant operational improvements through AI implementation, with many reporting substantial reductions in claim processing time and improved cash flow management.
Physician practice segment shows strong growth potential as smaller healthcare organizations recognize the benefits of AI billing automation. This category is particularly interested in cloud-based solutions that offer affordability, ease of implementation, and minimal IT infrastructure requirements. Specialty practices are increasingly adopting AI solutions tailored to their specific billing requirements and regulatory compliance needs.
Technology category analysis reveals that machine learning solutions are experiencing the highest adoption rates due to their versatility and proven effectiveness in various billing applications. Natural language processing technologies are gaining traction for automated medical coding, while robotic process automation is popular for routine task automation. Integration capabilities are becoming increasingly important across all technology categories as healthcare organizations seek seamless workflow automation.
Application-specific insights show that claims processing automation generates the highest return on investment for most healthcare organizations, followed by denial management and medical coding applications. Organizations are increasingly seeking comprehensive AI platforms that address multiple billing functions rather than point solutions for individual processes. Predictive analytics capabilities are becoming standard requirements as healthcare organizations seek to proactively identify and address potential billing issues before they impact revenue.
Healthcare organizations implementing AI billing solutions experience substantial operational and financial benefits that justify technology investments and drive continued market growth. Primary benefits include significant reductions in administrative costs, improved cash flow through faster claim processing, and enhanced accuracy that reduces costly claim denials and rework. Operational efficiency improvements enable healthcare staff to focus on patient care rather than administrative tasks, contributing to improved job satisfaction and reduced turnover in billing departments.
Financial performance improvements are measurable and substantial, with organizations typically experiencing faster payment cycles, reduced days in accounts receivable, and improved collection rates. AI solutions provide enhanced visibility into revenue cycle performance through advanced analytics and reporting capabilities, enabling data-driven decision-making and continuous process improvement. Compliance benefits include automated regulatory updates, reduced audit risks, and improved documentation accuracy that supports quality reporting requirements.
Technology vendors benefit from expanding market opportunities, recurring revenue streams through subscription-based models, and opportunities for strategic partnerships with healthcare organizations. The growing demand for AI billing solutions creates opportunities for innovation, market differentiation, and expansion into new healthcare segments and geographic markets. Competitive advantages can be achieved through specialized functionality, superior integration capabilities, and demonstrated return on investment for customers.
Patients ultimately benefit from AI billing implementations through improved billing accuracy, faster processing times, and enhanced transparency in healthcare financial transactions. AI solutions can improve patient financial experience through automated payment options, clearer billing communications, and reduced billing errors that cause patient confusion and dissatisfaction. Healthcare accessibility may improve as operational efficiencies enable healthcare organizations to allocate more resources to patient care and service expansion.
Strengths:
Weaknesses:
Opportunities:
Threats:
Automation acceleration represents the most significant trend in the AI medical billing market, with healthcare organizations increasingly seeking comprehensive automation solutions that address entire billing workflows rather than individual processes. This trend is driving demand for integrated platforms that combine multiple AI technologies and provide end-to-end billing automation capabilities. Intelligent automation is evolving beyond simple task automation to include predictive capabilities and proactive problem resolution.
Cloud-first strategies are becoming predominant as healthcare organizations recognize the benefits of cloud-based AI solutions including reduced infrastructure costs, improved scalability, and enhanced accessibility. Cloud deployment models enable smaller healthcare organizations to access advanced AI capabilities without substantial upfront investments. Software-as-a-Service models are particularly popular, providing predictable costs and continuous feature updates.
Real-time processing capabilities are increasingly important as healthcare organizations seek to accelerate cash flow and improve operational efficiency. AI solutions that provide instant claim validation, real-time denial alerts, and immediate payment processing are gaining market preference. Mobile accessibility is also becoming standard as healthcare professionals require access to billing information and capabilities from various devices and locations.
Advanced analytics integration is transforming AI billing solutions from operational tools to strategic platforms that provide insights for business optimization. Healthcare organizations are seeking AI solutions that offer predictive analytics, performance benchmarking, and strategic recommendations for revenue cycle improvement. Artificial intelligence is evolving to provide more sophisticated decision-making capabilities and autonomous problem resolution, with some organizations reporting automated resolution rates exceeding 80% for routine billing issues.
Strategic acquisitions and partnerships are reshaping the competitive landscape as established healthcare technology companies acquire AI specialists to enhance their billing capabilities. These consolidation activities are creating more comprehensive solution offerings and accelerating technology development cycles. Major EHR vendors are particularly active in acquiring AI billing companies to integrate advanced automation capabilities into their platforms.
Regulatory developments including updated guidelines for AI use in healthcare and new interoperability requirements are influencing product development and market strategies. Healthcare organizations are increasingly requiring AI solutions that demonstrate compliance with evolving regulatory standards and provide audit trails for automated decisions. Government initiatives promoting healthcare technology adoption are creating favorable market conditions and funding opportunities.
Technology innovations continue to advance AI capabilities in medical billing, with recent developments including improved natural language processing for clinical documentation, enhanced machine learning algorithms for predictive analytics, and advanced integration capabilities for seamless workflow automation. Emerging technologies such as blockchain for secure transactions and IoT for automated data collection are beginning to integrate with AI billing solutions.
Market expansion activities by leading vendors include international expansion, development of specialized solutions for niche healthcare markets, and creation of partner ecosystems to extend market reach. MarkWide Research analysis indicates that vendor strategies are increasingly focused on providing comprehensive platforms rather than point solutions, reflecting customer preferences for integrated automation capabilities.
Healthcare organizations considering AI billing implementations should prioritize solutions that demonstrate clear return on investment, provide comprehensive integration capabilities, and offer scalable deployment options. Organizations should conduct thorough assessments of their current billing processes, data quality, and technical infrastructure before selecting AI solutions. Pilot implementations are recommended to validate technology effectiveness and organizational readiness before full-scale deployment.
Technology vendors should focus on developing solutions that address specific healthcare billing challenges while providing flexibility for customization and integration with existing systems. Vendors should invest in customer success programs, comprehensive training resources, and ongoing support services to ensure successful implementations. Market differentiation should focus on proven outcomes, specialized functionality, and superior customer experience rather than generic AI capabilities.
Investment strategies should consider the long-term growth potential of the AI medical billing market while recognizing the importance of technology innovation and customer success in achieving sustainable competitive advantages. Investors should evaluate vendors based on their technology capabilities, market positioning, customer satisfaction, and ability to adapt to evolving healthcare requirements. Due diligence should include assessment of regulatory compliance, data security measures, and scalability potential.
Strategic partnerships between healthcare organizations and technology vendors can accelerate adoption and ensure successful implementations through collaborative development and shared expertise. Healthcare organizations should seek vendors that demonstrate commitment to long-term partnerships and continuous innovation. Vendor selection should prioritize companies with proven healthcare expertise, strong financial stability, and comprehensive support capabilities.
Market trajectory indicates continued robust growth in the AI medical billing market, driven by increasing healthcare digitization, regulatory requirements, and demonstrated return on investment from early adopters. The market is expected to experience accelerated adoption as AI technologies become more sophisticated, affordable, and accessible to healthcare organizations of all sizes. Technology evolution will continue to enhance AI capabilities, with emerging features including autonomous billing operations, predictive revenue optimization, and intelligent patient financial engagement.
Industry transformation is expected as AI billing solutions become standard components of healthcare technology infrastructure rather than optional enhancements. This transformation will drive consolidation among technology vendors and create opportunities for specialized AI companies to establish market leadership in niche segments. Integration trends will continue toward comprehensive platforms that combine AI billing with other healthcare technologies including EHR systems, patient engagement tools, and population health management solutions.
Global expansion opportunities will drive market growth as healthcare systems worldwide recognize the benefits of AI billing automation. Emerging markets present particularly attractive opportunities for vendors that can develop solutions tailored to local regulatory requirements and operational constraints. MWR projections suggest that international markets will contribute increasingly to overall market growth as healthcare digitization accelerates globally.
Innovation focus will shift toward more sophisticated AI capabilities including autonomous decision-making, advanced predictive analytics, and intelligent workflow optimization. Healthcare organizations will increasingly expect AI solutions to provide strategic insights and recommendations rather than simply automating existing processes. Market maturity will be characterized by standardized implementation methodologies, proven best practices, and measurable outcomes that demonstrate the value of AI billing investments, with industry-wide adoption rates projected to exceed 75% within the next five years.
The AI in medical billing market represents a transformative force in healthcare operations, offering substantial opportunities for improved efficiency, accuracy, and financial performance across healthcare organizations of all sizes. The market’s robust growth trajectory reflects the healthcare industry’s recognition of AI’s potential to address longstanding challenges in revenue cycle management while enabling organizations to focus resources on patient care rather than administrative burdens.
Market dynamics indicate a mature and rapidly evolving ecosystem with established technology leaders, innovative specialists, and emerging solutions that continue to push the boundaries of what’s possible in healthcare billing automation. The combination of proven return on investment, regulatory support, and technological advancement creates favorable conditions for continued market expansion and innovation.
Strategic implications for healthcare organizations include the need to develop comprehensive AI adoption strategies that align with operational goals, financial constraints, and technical capabilities. Organizations that successfully implement AI billing solutions position themselves for competitive advantages through improved operational efficiency, enhanced financial performance, and better patient experiences.
Future success in the AI medical billing market will depend on vendors’ ability to deliver measurable value, healthcare organizations’ commitment to digital transformation, and the industry’s collective efforts to address implementation challenges and maximize the benefits of artificial intelligence in healthcare operations. MarkWide Research analysis suggests that the market will continue to evolve toward more sophisticated, integrated solutions that transform healthcare billing from a necessary administrative function into a strategic advantage for healthcare organizations worldwide.
What is AI In Medical Billing?
AI in medical billing refers to the use of artificial intelligence technologies to automate and enhance the processes involved in medical billing, including coding, claims processing, and revenue cycle management.
What are the key companies in the AI In Medical Billing Market?
Key companies in the AI in medical billing market include Optum, Change Healthcare, and Cerner, which provide innovative solutions to streamline billing processes and improve accuracy, among others.
What are the growth factors driving the AI In Medical Billing Market?
The growth of the AI in medical billing market is driven by the increasing demand for automation in healthcare, the need for reducing billing errors, and the rising complexity of medical billing regulations.
What challenges does the AI In Medical Billing Market face?
Challenges in the AI in medical billing market include data privacy concerns, the need for integration with existing systems, and the potential for job displacement among billing professionals.
What future opportunities exist in the AI In Medical Billing Market?
Future opportunities in the AI in medical billing market include advancements in machine learning algorithms, the potential for personalized billing solutions, and the expansion of telehealth services requiring efficient billing practices.
What trends are shaping the AI In Medical Billing Market?
Trends shaping the AI in medical billing market include the increasing adoption of cloud-based solutions, the integration of AI with electronic health records, and the growing emphasis on patient-centric billing practices.
AI In Medical Billing Market
| Segmentation Details | Description |
|---|---|
| Product Type | Cloud-Based Solutions, On-Premise Solutions, Hybrid Solutions, Software as a Service |
| End User | Hospitals, Clinics, Diagnostic Centers, Billing Companies |
| Technology | Machine Learning, Natural Language Processing, Robotic Process Automation, Blockchain |
| Application | Claims Management, Payment Processing, Revenue Cycle Management, Fraud Detection |
Please note: The segmentation can be entirely customized to align with our client’s needs.
Leading companies in the AI In Medical Billing Market
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
North America
o US
o Canada
o Mexico
Europe
o Germany
o Italy
o France
o UK
o Spain
o Denmark
o Sweden
o Austria
o Belgium
o Finland
o Turkey
o Poland
o Russia
o Greece
o Switzerland
o Netherlands
o Norway
o Portugal
o Rest of Europe
Asia Pacific
o China
o Japan
o India
o South Korea
o Indonesia
o Malaysia
o Kazakhstan
o Taiwan
o Vietnam
o Thailand
o Philippines
o Singapore
o Australia
o New Zealand
o Rest of Asia Pacific
South America
o Brazil
o Argentina
o Colombia
o Chile
o Peru
o Rest of South America
The Middle East & Africa
o Saudi Arabia
o UAE
o Qatar
o South Africa
o Israel
o Kuwait
o Oman
o North Africa
o West Africa
o Rest of MEA
Trusted by Global Leaders
Fortune 500 companies, SMEs, and top institutions rely on MWR’s insights to make informed decisions and drive growth.
ISO & IAF Certified
Our certifications reflect a commitment to accuracy, reliability, and high-quality market intelligence trusted worldwide.
Customized Insights
Every report is tailored to your business, offering actionable recommendations to boost growth and competitiveness.
Multi-Language Support
Final reports are delivered in English and major global languages including French, German, Spanish, Italian, Portuguese, Chinese, Japanese, Korean, Arabic, Russian, and more.
Unlimited User Access
Corporate License offers unrestricted access for your entire organization at no extra cost.
Free Company Inclusion
We add 3–4 extra companies of your choice for more relevant competitive analysis — free of charge.
Post-Sale Assistance
Dedicated account managers provide unlimited support, handling queries and customization even after delivery.
GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at