444 Alaska Avenue
Suite #BAA205 Torrance, CA 90503 USA
+1 424 999 9627
24/7 Customer Support
sales@markwideresearch.com
Email us at
Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at
Corporate User License
Unlimited User Access, Post-Sale Support, Free Updates, Reports in English & Major Languages, and more
$3450
Market Overview
The value-based care payment market has witnessed significant growth in recent years, driven by the need for healthcare systems to shift from volume-based reimbursement models to value-based models. Value-based care payment models aim to improve the quality and outcomes of healthcare services while controlling costs. This comprehensive analysis delves into the key insights, trends, and dynamics of the value-based care payment market.
Meaning
Value-based care payment refers to a healthcare payment model that focuses on the value delivered to patients rather than the quantity of services provided. Under this model, healthcare providers are incentivized to deliver high-quality care, improve patient outcomes, and reduce costs. Payment is tied to performance metrics, such as patient satisfaction, clinical outcomes, and cost-effectiveness, fostering a more patient-centered approach to healthcare delivery.
Executive Summary
The value-based care payment market has experienced significant growth due to the increasing recognition of the limitations of fee-for-service models. This analysis provides an in-depth understanding of the market, its drivers, restraints, and opportunities. Additionally, it explores the regional analysis, competitive landscape, segmentation, key trends, COVID-19 impact, industry developments, and offers future outlook and conclusions.
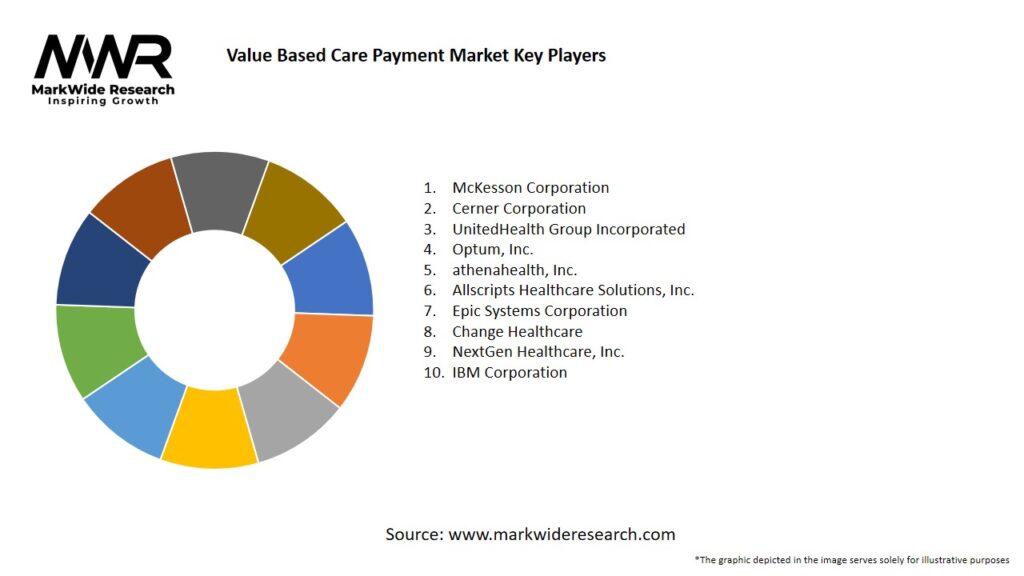
Important Note: The companies listed in the image above are for reference only. The final study will cover 18–20 key players in this market, and the list can be adjusted based on our client’s requirements.
Key Market Insights
Market Drivers
Market Restraints
Market Opportunities
Market Dynamics
The value-based care payment market is characterized by dynamic factors that influence its growth and evolution. These dynamics include changing healthcare policies, evolving payment models, technological advancements, shifting patient expectations, and the increasing focus on population health management. Understanding these dynamics is crucial for stakeholders to navigate the market landscape successfully.
Regional Analysis
The value-based care payment market exhibits regional variations due to differences in healthcare systems, policies, and infrastructure. This analysis provides an in-depth assessment of regional markets, including North America, Europe, Asia Pacific, and Latin America. It explores market trends, regulatory landscapes, key players, and growth opportunities in each region.
Competitive Landscape
Leading companies in the Value Based Care Payment Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
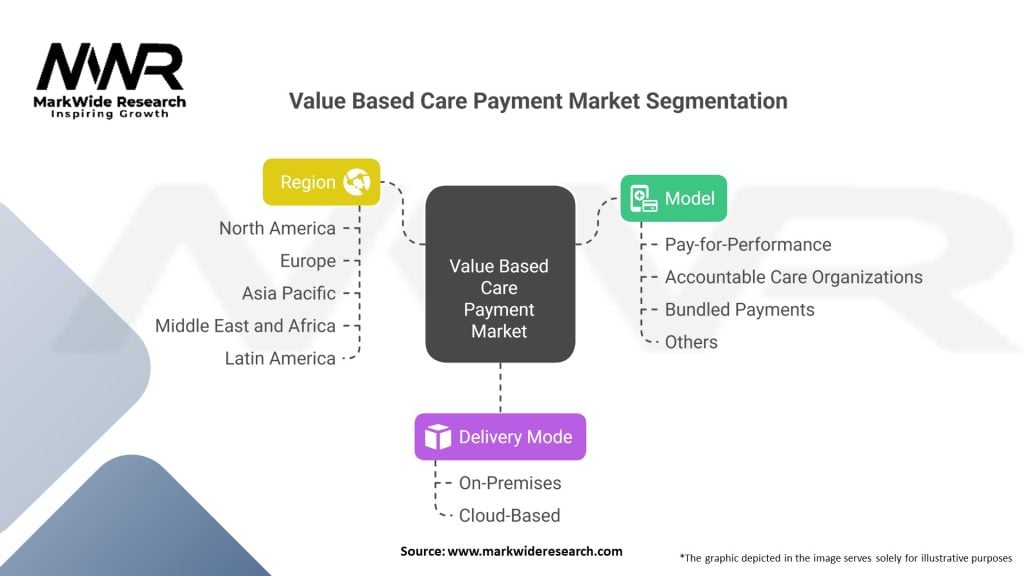
Segmentation
The value-based care payment market can be segmented based on payment models, healthcare settings, and end-users. This analysis examines each segment in detail, highlighting their market size, growth prospects, and key trends. By understanding the different segments, stakeholders can tailor their strategies and offerings to meet specific market needs.
Category-wise Insights
This section provides category-wise insights into the value-based care payment market, covering areas such as bundled payments, pay-for-performance models, accountable care organizations (ACOs), and capitation. It explores the adoption rates, benefits, challenges, and future prospects of each category, offering a comprehensive understanding of the market dynamics.
Key Benefits for Industry Participants and Stakeholders
SWOT Analysis
Market Key Trends
Covid-19 Impact
The COVID-19 pandemic has significantly impacted the healthcare industry, including the value-based care payment market. This analysis assesses the short-term and long-term effects of the pandemic on value-based care initiatives, highlighting the challenges faced by stakeholders and the strategies employed to mitigate the impact.
Key Industry Developments
This section provides an overview of recent industry developments, including mergers and acquisitions, partnerships, product launches, and regulatory updates. These developments influence the market landscape and shape the future direction of value-based care payment models.
Analyst Suggestions
Based on the analysis and market trends, industry experts provide suggestions and recommendations for stakeholders. These suggestions aim to assist healthcare providers, payers, policymakers, and technology vendors in effectively implementing and maximizing the benefits of value-based care payment models.
Future Outlook
The value-based care payment market is poised for significant growth in the coming years. This section offers insights into the market’s future prospects, including emerging trends, growth opportunities, and potential challenges. It helps stakeholders anticipate market developments and strategize for future success.
Conclusion
The value-based care payment market presents a transformative approach to healthcare delivery and payment. By focusing on value, quality, and patient outcomes, value-based care models aim to improve healthcare effectiveness, efficiency, and patient satisfaction. This analysis provides a comprehensive understanding of the market, empowering stakeholders to make informed decisions, implement effective strategies, and contribute to the advancement of value-based care initiatives.
Value Based Care Payment Market
| Segmentation | Details |
|---|---|
| Model | Pay-for-Performance, Accountable Care Organizations, Bundled Payments, Others |
| Delivery Mode | On-Premises, Cloud-Based |
| Region | North America, Europe, Asia Pacific, Middle East and Africa, Latin America |
Please note: The segmentation can be entirely customized to align with our client’s needs.
Leading companies in the Value Based Care Payment Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
North America
o US
o Canada
o Mexico
Europe
o Germany
o Italy
o France
o UK
o Spain
o Denmark
o Sweden
o Austria
o Belgium
o Finland
o Turkey
o Poland
o Russia
o Greece
o Switzerland
o Netherlands
o Norway
o Portugal
o Rest of Europe
Asia Pacific
o China
o Japan
o India
o South Korea
o Indonesia
o Malaysia
o Kazakhstan
o Taiwan
o Vietnam
o Thailand
o Philippines
o Singapore
o Australia
o New Zealand
o Rest of Asia Pacific
South America
o Brazil
o Argentina
o Colombia
o Chile
o Peru
o Rest of South America
The Middle East & Africa
o Saudi Arabia
o UAE
o Qatar
o South Africa
o Israel
o Kuwait
o Oman
o North Africa
o West Africa
o Rest of MEA
Trusted by Global Leaders
Fortune 500 companies, SMEs, and top institutions rely on MWR’s insights to make informed decisions and drive growth.
ISO & IAF Certified
Our certifications reflect a commitment to accuracy, reliability, and high-quality market intelligence trusted worldwide.
Customized Insights
Every report is tailored to your business, offering actionable recommendations to boost growth and competitiveness.
Multi-Language Support
Final reports are delivered in English and major global languages including French, German, Spanish, Italian, Portuguese, Chinese, Japanese, Korean, Arabic, Russian, and more.
Unlimited User Access
Corporate License offers unrestricted access for your entire organization at no extra cost.
Free Company Inclusion
We add 3–4 extra companies of your choice for more relevant competitive analysis — free of charge.
Post-Sale Assistance
Dedicated account managers provide unlimited support, handling queries and customization even after delivery.
GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at