444 Alaska Avenue
Suite #BAA205 Torrance, CA 90503 USA
+1 424 999 9627
24/7 Customer Support
sales@markwideresearch.com
Email us at
Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at
Corporate User License
Unlimited User Access, Post-Sale Support, Free Updates, Reports in English & Major Languages, and more
$2450
Market Overview
The US Colonic Stents Market is witnessing steady growth driven by the rising prevalence of colorectal cancer, gastrointestinal obstructions, and other colorectal disorders requiring palliative care interventions. Colonic stents are medical devices used in endoscopic procedures to relieve colonic obstruction, restore bowel function, and alleviate symptoms in patients with malignant or benign colorectal strictures. With advancements in stent technology, minimally invasive techniques, and endoscopic interventions, the US colonic stents market offers opportunities for manufacturers, healthcare providers, and patients to improve treatment outcomes, enhance quality of life, and reduce morbidity associated with colorectal diseases.
Meaning
Colonic stents, also known as self-expandable metal stents (SEMS), are tubular medical devices made of biocompatible materials such as nitinol or stainless steel that can be inserted into the colon endoscopically to relieve mechanical obstruction, maintain luminal patency, and facilitate bowel decompression in patients with colorectal strictures caused by tumors, adhesions, or inflammatory conditions. Colonic stenting is a minimally invasive alternative to surgical resection for palliative care, symptom relief, and bridging to definitive treatment in patients with advanced colorectal cancer, bowel obstruction, or refractory disease, offering benefits such as rapid relief of symptoms, shorter hospital stays, and improved quality of life.
Executive Summary
The US Colonic Stents Market is experiencing growth driven by the increasing incidence of colorectal cancer, gastrointestinal diseases, and inflammatory bowel conditions necessitating palliative interventions to relieve colonic obstruction, alleviate symptoms, and improve patient outcomes. This market presents opportunities for manufacturers, healthcare providers, and patients to access innovative stent technologies, expand treatment options, and optimize clinical management strategies for colorectal disorders. However, challenges such as procedural complications, device-related adverse events, and healthcare disparities need to be addressed to ensure safe, effective, and equitable access to colonic stenting for patients across the United States.
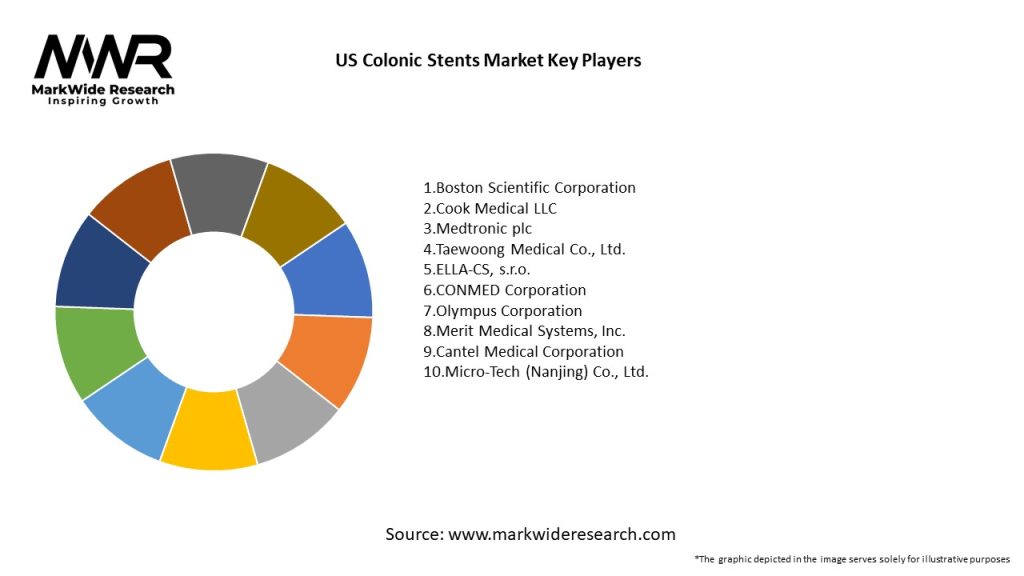
Important Note: The companies listed in the image above are for reference only. The final study will cover 18–20 key players in this market, and the list can be adjusted based on our client’s requirements.
Key Market Insights
Market Drivers
Market Restraints
Market Opportunities

Market Dynamics
The US Colonic Stents Market operates in a dynamic healthcare landscape influenced by factors such as technological innovations, regulatory reforms, reimbursement policies, and patient preferences that shape market trends, clinical practices, and healthcare delivery models for colorectal disorders requiring palliative interventions with colonic stenting as a minimally invasive treatment option.
Regional Analysis
The US Colonic Stents Market exhibits regional variations in clinical practice patterns, healthcare infrastructure, and patient outcomes influenced by factors such as population demographics, disease epidemiology, and healthcare utilization rates that impact the availability, accessibility, and affordability of colonic stenting services in different states, cities, and geographic regions across the United States.
Competitive Landscape
Leading Companies in the US Colonic Stents Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
Segmentation
The US Colonic Stents Market can be segmented based on various factors such as product type, material composition, indication, end-user segment, and geographic region that enable stakeholders to analyze market trends, target specific patient populations, and tailor clinical management strategies, research protocols, and healthcare interventions to meet the diverse needs and preferences of colorectal cancer patients requiring palliative care interventions with colonic stenting.
Category-wise Insights
Key Benefits for Industry Participants and Stakeholders
The US Colonic Stents Market offers several benefits for industry participants and stakeholders, including medical device manufacturers, healthcare providers, patients, and caregivers that include:
SWOT Analysis
A SWOT analysis of the US Colonic Stents Market provides insights into the market’s strengths, weaknesses, opportunities, and threats, enabling stakeholders to formulate strategies, mitigate risks, and capitalize on market dynamics to achieve competitive advantage, market leadership, and sustainable growth in the colorectal oncology sector.
Market Key Trends
Covid-19 Impact
The COVID-19 pandemic has had a significant impact on the US Colonic Stents Market, affecting patient access to healthcare services, procedural volumes, and clinical outcomes associated with colorectal cancer management, gastrointestinal disorders, and palliative care interventions requiring colonic stenting as an essential treatment option to alleviate symptoms, maintain bowel function, and improve quality of life in patients with advanced or metastatic disease.
Key Industry Developments
Analyst Suggestions
Future Outlook
The US Colonic Stents Market is poised for sustained growth driven by factors such as population demographics, disease epidemiology, technological innovations, and healthcare reforms that shape demand patterns, treatment paradigms, and market opportunities for manufacturers, suppliers, and healthcare providers to meet evolving patient needs, address clinical challenges, and improve outcomes in the colorectal oncology sector.
Conclusion
The US Colonic Stents Market presents significant opportunities for manufacturers, healthcare providers, and patients to access innovative technologies, expand treatment options, and optimize clinical management strategies for colorectal disorders requiring palliative interventions with colonic stenting as a minimally invasive treatment option to alleviate symptoms, improve quality of life, and enhance patient outcomes in diverse clinical settings across the United States. By embracing technological advancements, quality improvement initiatives, and research collaborations, stakeholders can navigate market challenges, capitalize on emerging trends, and achieve sustainable growth, clinical excellence, and patient-centered care in the colorectal oncology sector.
What is Colonic Stents?
Colonic stents are medical devices used to treat obstructions in the colon. They are designed to be placed within the colon to keep it open, allowing for the passage of stool and reducing the risk of complications associated with bowel obstructions.
What are the key players in the US Colonic Stents Market?
Key players in the US Colonic Stents Market include Boston Scientific, Medtronic, Cook Medical, and Abbott Laboratories, among others. These companies are involved in the development and manufacturing of innovative stenting solutions for gastrointestinal applications.
What are the growth factors driving the US Colonic Stents Market?
The growth of the US Colonic Stents Market is driven by factors such as the increasing prevalence of colorectal cancer, advancements in minimally invasive surgical techniques, and a growing aging population that is more susceptible to gastrointestinal disorders.
What challenges does the US Colonic Stents Market face?
The US Colonic Stents Market faces challenges such as the risk of complications associated with stent placement, high costs of advanced stenting technologies, and regulatory hurdles that can delay product approvals.
What opportunities exist in the US Colonic Stents Market?
Opportunities in the US Colonic Stents Market include the development of biodegradable stents, increasing demand for personalized medicine, and the potential for expanding applications in treating various gastrointestinal conditions.
What trends are shaping the US Colonic Stents Market?
Trends in the US Colonic Stents Market include the rise of hybrid stenting techniques, the integration of smart technology in stents for better monitoring, and a focus on patient-centered care that emphasizes minimally invasive procedures.
US Colonic Stents Market
| Segmentation Details | Description |
|---|---|
| Product Type | Self-Expanding Stents, Balloon-Expandable Stents, Covered Stents, Uncovered Stents |
| Material | Metal, Polymer, Hybrid, Biodegradable |
| End User | Hospitals, Ambulatory Surgical Centers, Specialty Clinics, Research Institutions |
| Application | Colorectal Cancer, Inflammatory Bowel Disease, Diverticulitis, Others |
Please note: The segmentation can be entirely customized to align with our client’s needs.
Leading Companies in the US Colonic Stents Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
Trusted by Global Leaders
Fortune 500 companies, SMEs, and top institutions rely on MWR’s insights to make informed decisions and drive growth.
ISO & IAF Certified
Our certifications reflect a commitment to accuracy, reliability, and high-quality market intelligence trusted worldwide.
Customized Insights
Every report is tailored to your business, offering actionable recommendations to boost growth and competitiveness.
Multi-Language Support
Final reports are delivered in English and major global languages including French, German, Spanish, Italian, Portuguese, Chinese, Japanese, Korean, Arabic, Russian, and more.
Unlimited User Access
Corporate License offers unrestricted access for your entire organization at no extra cost.
Free Company Inclusion
We add 3–4 extra companies of your choice for more relevant competitive analysis — free of charge.
Post-Sale Assistance
Dedicated account managers provide unlimited support, handling queries and customization even after delivery.
GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at