444 Alaska Avenue
Suite #BAA205 Torrance, CA 90503 USA
+1 424 999 9627
24/7 Customer Support
sales@markwideresearch.com
Email us at
Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at
Corporate User License
Unlimited User Access, Post-Sale Support, Free Updates, Reports in English & Major Languages, and more
$3450
The healthcare reimbursement market plays a vital role in the healthcare industry by providing a framework for the financial aspects of medical services. It involves the process of compensating healthcare providers for the services they render to patients. This market encompasses various reimbursement models, such as fee-for-service, value-based reimbursement, bundled payments, and capitation. In this analysis, we will delve into the key aspects of the healthcare reimbursement market, exploring its meaning, market dynamics, regional analysis, competitive landscape, segmentation, industry developments, and future outlook.
Healthcare reimbursement refers to the compensation healthcare providers receive for the services they deliver. It involves the payment structure, policies, and procedures that govern the financial aspect of healthcare delivery. Reimbursement models aim to strike a balance between providing quality care and ensuring fair compensation for healthcare providers.
Executive Summary
The healthcare reimbursement market has experienced significant growth in recent years. With the ever-increasing demand for healthcare services, reimbursement models have become essential for sustaining the industry. This analysis provides an in-depth understanding of the market, highlighting key insights, market drivers, restraints, opportunities, and market dynamics that shape the reimbursement landscape.

Important Note: The companies listed in the image above are for reference only. The final study will cover 18–20 key players in this market, and the list can be adjusted based on our client’s requirements.
Key Market Insights
Market Drivers
Market Restraints
Market Opportunities
Market Dynamics
The healthcare reimbursement market is characterized by continuous evolution and adaptation. The dynamics within the market are influenced by several factors, including technological advancements, changing regulations, shifting patient expectations, and market competition. It is essential for stakeholders to remain agile and proactive in response to these dynamics to ensure efficient and sustainable reimbursement practices.
Regional Analysis
The healthcare reimbursement market varies across different regions due to variations in healthcare systems, regulatory frameworks, and cultural factors. Regional analysis helps identify market trends, reimbursement practices, and opportunities unique to specific geographical areas. It enables stakeholders to understand the local dynamics and tailor their reimbursement strategies accordingly.
Competitive Landscape
Leading Companies in the Healthcare Reimbursement Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
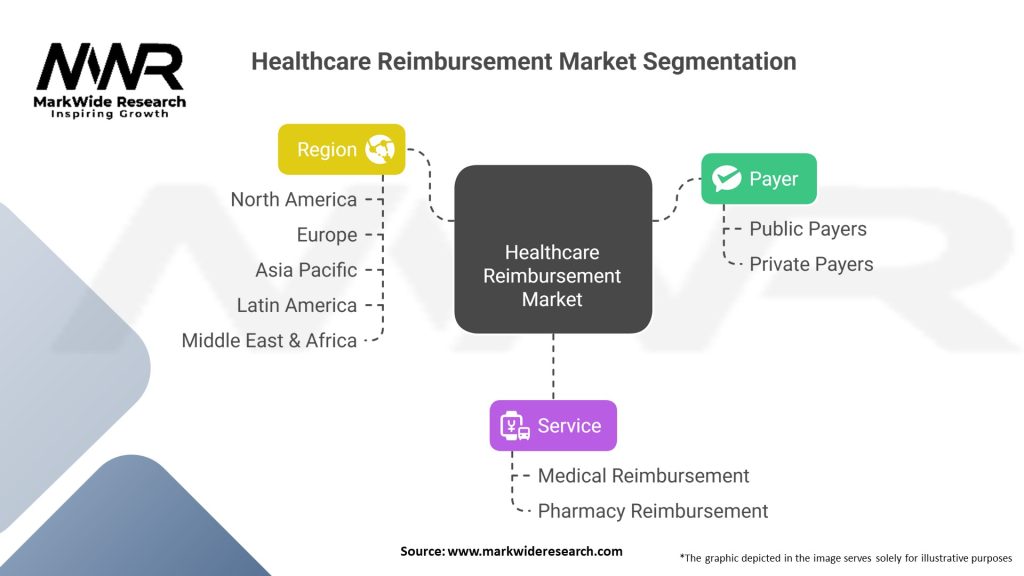
Segmentation
The healthcare reimbursement market can be segmented based on various factors, including reimbursement model, healthcare sector, and geography. By understanding the distinct segments within the market, stakeholders can tailor their strategies to address specific needs and challenges. Segmentation enables a focused approach in designing reimbursement policies and improving overall market efficiency.
Category-wise Insights
To gain a comprehensive understanding of the healthcare reimbursement market, it is crucial to examine it from different perspectives. Category-wise insights provide a deeper analysis of specific aspects, such as reimbursement models (fee-for-service, value-based reimbursement), healthcare sectors (hospitals, clinics, long-term care facilities), and payer types (public, private, self-insured). These insights shed light on the nuances and complexities within each category, guiding decision-making processes for stakeholders.
Key Benefits for Industry Participants and Stakeholders
Industry participants and stakeholders in the healthcare reimbursement market can reap several benefits from effective reimbursement practices. These include:
SWOT Analysis
Strengths:
Essential Component of Healthcare: Reimbursement systems are critical for the financial sustainability of healthcare providers.
Regulatory Frameworks: Established guidelines and policies provide a structured environment for reimbursement processes.
Data-Driven Improvements: Advances in health informatics and analytics enhance reimbursement accuracy and efficiency.
Weaknesses:
Complex and Time-Consuming Processes: Bureaucratic and often cumbersome procedures can delay reimbursements and increase administrative burdens.
Inconsistent Policies: Variability in reimbursement policies across regions and payers may lead to inefficiencies.
Cost Pressures: Rising healthcare costs challenge the sustainability of current reimbursement models.
Opportunities:
Technological Integration: Implementation of digital solutions and automated systems can streamline reimbursement processes.
Policy Reforms: Regulatory initiatives aimed at simplifying reimbursement systems can improve efficiency.
Expansion of Telehealth: Growing telemedicine services create new reimbursement models and opportunities for innovation.
Threats:
Regulatory Uncertainty: Changes in government policies and healthcare regulations can disrupt reimbursement frameworks.
Economic Pressures: Budget constraints and cost-cutting measures in healthcare systems may lead to lower reimbursement rates.
Market Competition: Increased competition among healthcare providers can drive down reimbursement margins.
Market Key Trends
Several key trends are shaping the healthcare reimbursement market:
Covid-19 Impact
The COVID-19 pandemic has had a significant impact on the healthcare reimbursement market. The rapid adoption of telehealth services, changes in reimbursement policies to accommodate virtual care, and the financial strain on healthcare systems due to increased demand for services have reshaped the reimbursement landscape. COVID-19 has highlighted the importance of flexibility and adaptability in reimbursement models to meet evolving healthcare needs.
Key Industry Developments
The healthcare reimbursement market is witnessing various industry developments:
Analyst Suggestions
Based on the analysis of the healthcare reimbursement market, certain suggestions emerge:
Future Outlook
The future of the healthcare reimbursement market appears promising, with several trends and developments shaping its trajectory. The shift towards value-based reimbursement models is expected to continue, incentivizing quality improvement and patient-centered care. Advancements in technology will further streamline reimbursement processes, enhance data analytics capabilities, and enable more accurate and efficient claims processing.
The COVID-19 pandemic has accelerated the adoption of telehealth and virtual care, leading to an increased focus on reimbursement models that accommodate these services. Regulatory reforms, policy changes, and ongoing collaborations will shape the market’s future, with an emphasis on affordability, transparency, and improved patient outcomes.
Conclusion
The healthcare reimbursement market is a complex and dynamic landscape that plays a vital role in ensuring financial stability for healthcare providers and facilitating access to quality care for patients. This analysis has provided a comprehensive overview of the market, including its meaning, key insights, market drivers, restraints, opportunities, and market dynamics.
What is the Healthcare Reimbursement?
Healthcare reimbursement refers to the process by which healthcare providers are paid for their services by insurance companies or government programs. This system is crucial for ensuring that medical services are accessible and that providers are compensated for their work.
Who are the key players in the Healthcare Reimbursement Market?
Key players in the Healthcare Reimbursement Market include major insurance companies like UnitedHealth Group, Anthem, and Aetna, as well as government programs such as Medicare and Medicaid. These entities play significant roles in determining reimbursement rates and policies, among others.
What are the main drivers of growth in the Healthcare Reimbursement Market?
The growth of the Healthcare Reimbursement Market is driven by factors such as the increasing prevalence of chronic diseases, the rising costs of healthcare services, and the expansion of insurance coverage. Additionally, technological advancements in healthcare delivery are also contributing to market growth.
What challenges does the Healthcare Reimbursement Market face?
The Healthcare Reimbursement Market faces challenges such as regulatory changes, the complexity of billing processes, and issues related to fraud and abuse. These challenges can lead to delays in payments and increased administrative costs for healthcare providers.
What opportunities exist in the Healthcare Reimbursement Market?
Opportunities in the Healthcare Reimbursement Market include the adoption of value-based care models, which focus on patient outcomes rather than service volume. Additionally, the integration of telehealth services presents new avenues for reimbursement strategies.
What trends are shaping the Healthcare Reimbursement Market?
Trends in the Healthcare Reimbursement Market include the shift towards value-based reimbursement models, increased transparency in pricing, and the growing use of data analytics to improve reimbursement processes. These trends are reshaping how providers are compensated for their services.
Healthcare Reimbursement Market:
| Segmentation | Details |
|---|---|
| Payer | Public Payers, Private Payers |
| Service | Medical Reimbursement, Pharmacy Reimbursement |
| Region | North America, Europe, Asia Pacific, Latin America, Middle East & Africa |
Please note: The segmentation can be entirely customized to align with our client’s needs.
Leading Companies in the Healthcare Reimbursement Market:
Please note: This is a preliminary list; the final study will feature 18–20 leading companies in this market. The selection of companies in the final report can be customized based on our client’s specific requirements.
North America
o US
o Canada
o Mexico
Europe
o Germany
o Italy
o France
o UK
o Spain
o Denmark
o Sweden
o Austria
o Belgium
o Finland
o Turkey
o Poland
o Russia
o Greece
o Switzerland
o Netherlands
o Norway
o Portugal
o Rest of Europe
Asia Pacific
o China
o Japan
o India
o South Korea
o Indonesia
o Malaysia
o Kazakhstan
o Taiwan
o Vietnam
o Thailand
o Philippines
o Singapore
o Australia
o New Zealand
o Rest of Asia Pacific
South America
o Brazil
o Argentina
o Colombia
o Chile
o Peru
o Rest of South America
The Middle East & Africa
o Saudi Arabia
o UAE
o Qatar
o South Africa
o Israel
o Kuwait
o Oman
o North Africa
o West Africa
o Rest of MEA
Trusted by Global Leaders
Fortune 500 companies, SMEs, and top institutions rely on MWR’s insights to make informed decisions and drive growth.
ISO & IAF Certified
Our certifications reflect a commitment to accuracy, reliability, and high-quality market intelligence trusted worldwide.
Customized Insights
Every report is tailored to your business, offering actionable recommendations to boost growth and competitiveness.
Multi-Language Support
Final reports are delivered in English and major global languages including French, German, Spanish, Italian, Portuguese, Chinese, Japanese, Korean, Arabic, Russian, and more.
Unlimited User Access
Corporate License offers unrestricted access for your entire organization at no extra cost.
Free Company Inclusion
We add 3–4 extra companies of your choice for more relevant competitive analysis — free of charge.
Post-Sale Assistance
Dedicated account managers provide unlimited support, handling queries and customization even after delivery.
GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


GET A FREE SAMPLE REPORT
This free sample study provides a complete overview of the report, including executive summary, market segments, competitive analysis, country level analysis and more.
ISO AND IAF CERTIFIED


Suite #BAA205 Torrance, CA 90503 USA
24/7 Customer Support
Email us at